Why Understanding Continuum of Care Matters for Your Recovery Journey
Continuum of care refers to a comprehensive, coordinated system that provides seamless healthcare services across different levels and stages of treatment. This integrated approach ensures patients receive the right care at the right time, whether they’re starting with detox, moving through residential treatment, or transitioning to outpatient support.
Quick Answer: What is Continuum of Care?
- Comprehensive system – Covers all levels of care from prevention to long-term support
- Coordinated approach – Healthcare providers work together and share information
- Seamless transitions – Patients move smoothly between different treatment stages
- Personalized care – Treatment adapts to individual needs over time
- Multiple stages – Includes detox, residential, outpatient, and aftercare services
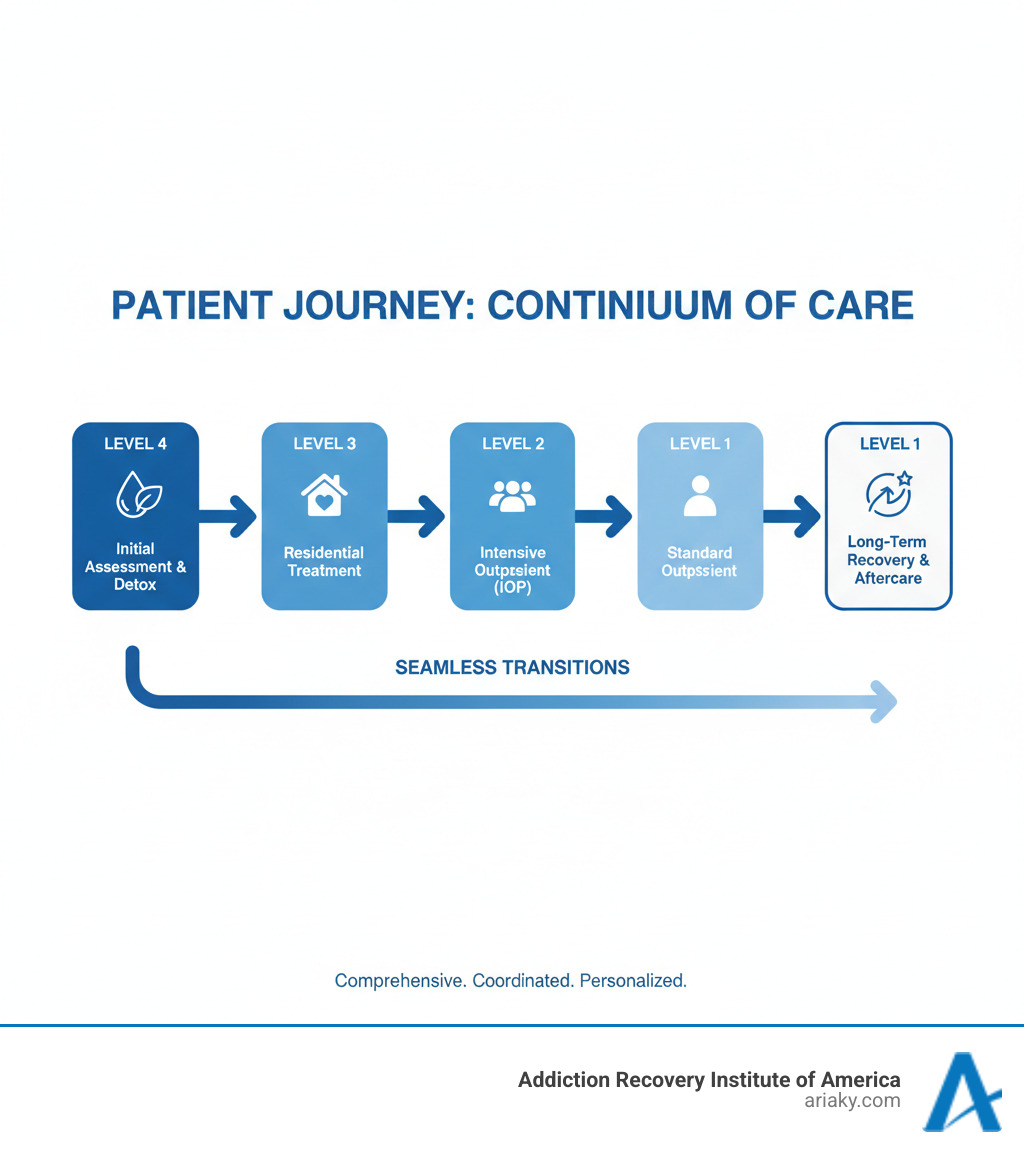
For addiction treatment specifically, the continuum starts with initial assessment and detoxification, progresses through residential or inpatient care, continues with outpatient programs, and extends to long-term recovery support. The goal is simple: provide uninterrupted care that reduces relapse risk and improves long-term outcomes.
Research shows that patients who follow a continuum of care model demonstrate significantly greater levels of improvement over time compared to those receiving fragmented care. This approach addresses the physical, emotional, and behavioral aspects of addiction through multiple interconnected services.
The beauty of this system lies in its flexibility. As your needs change during recovery, your care team adjusts the level of support accordingly. You might start with 24/7 medical supervision in detox, transition to intensive therapy in residential treatment, then gradually move to weekly outpatient sessions while rebuilding your life.
The Building Blocks: Core Components and Key Benefits
When we talk about the continuum of care, we’re describing a holistic system designed to guide and support individuals through their health journey. It’s like building a strong, reliable bridge that connects every stage of care, ensuring no one falls through the cracks. This isn’t just a nice-to-have; it’s essential for achieving lasting health and well-being.

Core Components of Care
At the heart of any effective continuum of care are several interconnected components that work in harmony:
- Personnel: This includes a diverse team of healthcare professionals like nurses, social workers, doctors, therapists, and support staff. Nurses, for instance, are the largest segment of healthcare workers in the United States, and globally, nurses and midwives comprised nearly 50% of the health care workforce in 2022. They play a pivotal role in care coordination, patient education, and advocacy, often being the consistent point of contact for patients. Social workers are vital for navigating complex social determinants of health and connecting patients with necessary resources.
- Facilities: These are the physical locations where care is delivered, ranging from hospitals and residential treatment centers to outpatient clinics, community health centers, and home care settings. The right facility at the right time is crucial for appropriate treatment.
- Procedures: This encompasses all medical, therapeutic, and diagnostic interventions applied throughout a patient’s journey, custom to their evolving needs.
- Treatments: These are the specific methods used to address health conditions, whether it’s medication-assisted treatment, individual therapy, group counseling, or specialized medical procedures.
- Communication: Perhaps the most critical component, effective communication ensures that all members of the care team, including the patient and their family, are informed and aligned. This prevents misunderstandings and ensures continuity.
- Data Sharing: Seamless and secure sharing of patient information across different providers and settings is fundamental. This allows for informed decision-making and avoids repetitive testing or conflicting treatments.
These components aren’t isolated; they’re constantly interacting, forming a dynamic system that adapts to each individual’s unique situation.
Benefits for Patients and Providers
The implementation of a robust continuum of care yields significant advantages for everyone involved:
For Patients:
- Improved Outcomes: Patients who follow a continuum of care show significantly greater levels of improvement over a 10-year period. Coordinated care leads to better health results, especially for chronic conditions or complex needs.
- Improved Safety: With consistent oversight and shared information, the risk of medication errors, missed appointments, or fragmented care leading to adverse events is significantly reduced.
- Personalized Care: The system is designed to be flexible, adapting to individual needs as they evolve. This means receiving care that is truly custom to your journey, not a one-size-fits-all approach.
- Greater Satisfaction: Patients who received coordinated care across various procedures reported greater satisfaction with the care they received for nine of the 13 types of care reviewed. Knowing that your care is managed and understood across different providers brings peace of mind.
- Seamless Transitions: Moving between different levels of care—say, from an inpatient program to an outpatient one—becomes a smooth process, reducing anxiety and ensuring continued support.
- Reduced Expense: By preventing crises, reducing readmissions, and optimizing resource use, a coordinated approach can ultimately lead to less overall cost for the patient and the healthcare system.
For Providers:
- Greater Efficiency: Streamlined processes, shared data, and clear communication reduce administrative burdens and allow providers to focus more on patient care.
- Better Reputation: Health systems known for their seamless, high-quality continuum of care attract more patients and build trust within the community.
- Improved Morale: Working within a well-coordinated system where patients thrive can boost staff satisfaction and reduce burnout.
- Increased Reimbursements: Many modern healthcare models, including value-based care, tie reimbursement to patient outcomes. A strong continuum of care can lead to better results and, consequently, increased financial viability for providers.
We believe that a well-structured continuum of care is a win-win, fostering better health for individuals and a more effective, sustainable healthcare system for all.
A Spectrum of Support: Continuum of Care Models in Action
The beauty of the continuum of care model lies in its adaptability. Think of it like a skilled craftsman’s toolbox – the same fundamental principles can be applied to create solutions for vastly different challenges. Whether someone needs general healthcare support, is battling addiction, struggling with mental health issues, or facing homelessness, the core idea remains the same: seamless, coordinated care that adapts as needs change.
General Healthcare and Aging
In general healthcare, the continuum of care is like having a trusted guide throughout your entire life journey. It starts before you’re even sick and continues until your final days, adapting to whatever life throws your way.
Preventive care kicks things off with regular check-ups, vaccinations, and screenings. It’s the healthcare equivalent of changing your car’s oil – small steps that prevent big problems later. Your primary care doctor becomes your healthcare quarterback, coordinating everything and knowing your complete health story.
When you need specialized expertise, the system smoothly connects you to specialists like cardiologists or oncologists. No one gets lost in the shuffle or has to start their story from scratch each time.
Rehabilitation services step in after injuries, surgeries, or illnesses, helping you regain your independence through physical therapy, occupational therapy, or speech therapy. It’s about getting back to being you again.
For those with chronic conditions or aging-related needs, long-term care provides ongoing support. This might mean home health services, assisted living, or skilled nursing facilities. As SantaFe Senior Living points out, this approach is especially valuable for seniors because they don’t need to uproot their lives every time their health needs change.
Finally, palliative and hospice care focus on comfort and quality of life when curative treatment is no longer the goal. It’s about dignity, peace, and supporting both patients and their families during the most challenging times.
Understanding the Continuum of Care in Addiction Treatment
When it comes to addiction, the continuum of care isn’t just helpful – it’s absolutely essential. Addiction is a complex, chronic condition, and recovery is a marathon, not a sprint. The journey requires different types of support at different stages, all working together seamlessly.
At ARIA Kentucky, we’ve built our entire approach around this principle. We understand that what works in week one of recovery might not be what someone needs in month six or year two.
The journey typically begins with detoxification programs, where medical professionals safely guide people through withdrawal. It’s like having a skilled navigator help you through the most dangerous part of the journey.
Residential treatment follows, offering an immersive, 24/7 supportive environment where people can focus entirely on healing. Think of it as a protective cocoon where change can happen safely.
Our Partial Hospitalization Program (PHP) serves as a bridge between residential care and the real world. People get comprehensive daily treatment but return home each evening, gradually rebuilding their connection to everyday life.
The Intensive Outpatient Program (IOP) provides significant therapeutic support while allowing people to maintain work, school, or family responsibilities. It’s about finding that balance between recovery and life.
Outpatient treatment continues the support with less frequent sessions, focusing on relapse prevention and integrating recovery skills into daily routines. The training wheels are coming off, but the support remains.
Aftercare and relapse prevention recognize that recovery doesn’t end when formal treatment does. We provide alumni programs, support groups, and ongoing counseling because we know that sustained sobriety requires sustained support.
Our comprehensive continuum of care in addiction treatment is specifically designed for people in Kentucky and beyond, with accredited, AODE-certified centers in Ashland, Bowling Green, Lexington, and Louisville. We make sure that quality, personalized treatment is always within reach.
Mental Health and Social Services
The continuum of care model shines just as brightly in mental health and social services, where vulnerable populations often need the most coordinated support.
In mental health care, the journey starts with early intervention and prevention efforts – catching problems before they become crises. Outpatient therapy provides the foundation, including individual counseling, group sessions, and our therapy programs that address the whole person, not just symptoms.
When someone needs more intensive help, inpatient hospitalization provides stabilization and intensive treatment in a safe environment. But the support doesn’t stop there – ongoing support through peer groups and community services helps maintain long-term mental wellness.
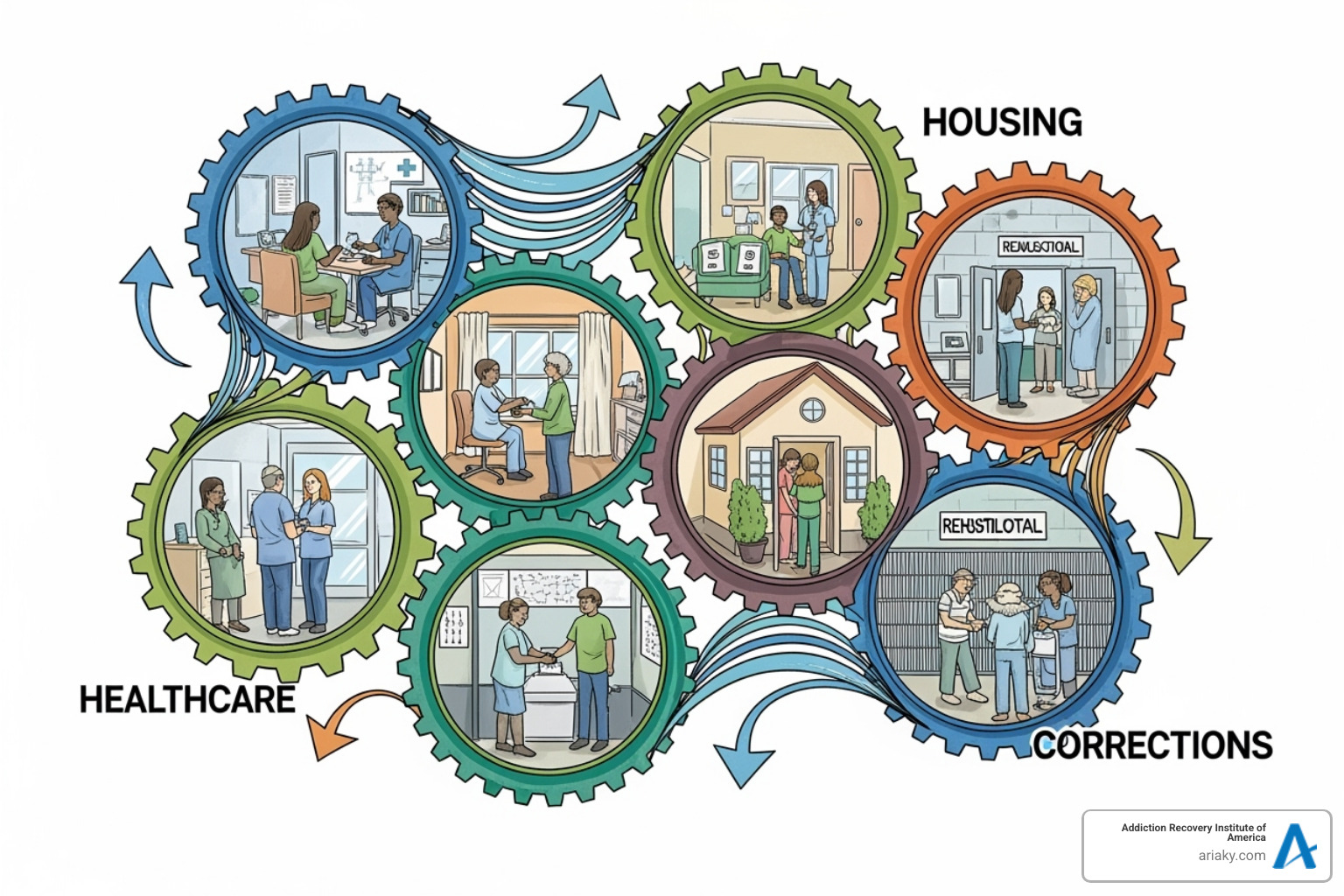
For people experiencing homelessness, the U.S. Department of Housing and Urban Development created the Continuum of Care Program specifically to address this complex challenge. It recognizes that homelessness isn’t just about lacking shelter – it’s about needing coordinated support across multiple areas.
The program starts with outreach and engagement to connect with people living on the streets. Emergency shelters provide immediate safety, while transitional housing offers temporary stability with supportive services to help people prepare for independence. Permanent supportive housing provides long-term assistance for those with chronic needs or disabilities.
What makes this approach so effective is its recognition that people experiencing homelessness often need help accessing mainstream programs like healthcare, employment services, and education. It’s not enough to just provide housing – people need comprehensive support to rebuild their lives.
These diverse applications prove that while the populations and challenges differ dramatically, the core philosophy remains the same: integrated, continuous, and adaptive support works. Whether someone is recovering from addiction, managing mental health challenges, or rebuilding their life after homelessness, the continuum of care model provides a roadmap for lasting change.
Building a Successful Continuum of Care Framework
Creating an effective continuum of care is like building a bridge that connects every stage of someone’s recovery journey. It’s not enough to simply have different services available – they need to work together like a well-coordinated team. This takes thoughtful planning, dedicated professionals, and the willingness to tackle some real challenges head-on.
The Role of Key Professionals
Behind every successful continuum of care are dedicated professionals who serve as the backbone of coordinated treatment. These aren’t just people doing their jobs – they’re the human connections that make seamless care possible.
Nurses often become the heart of care coordination. They’re the ones who get to know patients personally, understand their struggles, and help them steer the healthcare system. Think of them as your personal guides through what can feel like a confusing maze of appointments, treatments, and decisions. They build relationships, advocate for your needs, create comprehensive care plans, and make sure you’re connected to the right resources at the right time.
Social workers are the resource navigation experts who understand that recovery isn’t just about medical treatment. They know that housing, financial support, family dynamics, and community connections all play crucial roles in healing. These professionals help connect patients and families to social services, financial aid, housing assistance, and other community supports that create a foundation for lasting recovery.
Nurse practitioners bring a unique perspective to primary care, with 88% holding certifications in primary care and 70% actively delivering these services. They focus on whole-person care and often serve as the consistent point of contact throughout someone’s recovery journey. Their role in preventive care and long-term health management makes them essential coordinators within the continuum of care.
These professionals work alongside physicians, therapists, and specialists to create a comprehensive support network that adapts to each person’s changing needs.
Challenges and Barriers to Implementation
Let’s be honest – building an effective continuum of care isn’t easy. Even with the best intentions, several challenges can get in the way of seamless, integrated treatment.
Service integration is probably the biggest hurdle. Getting different healthcare providers, social services, and community organizations to truly work together is complex. Each organization has its own culture, priorities, and way of doing things. Breaking down these silos takes time and effort.
Funding issues create real barriers too. Traditional healthcare payment models often don’t reward the kind of preventive care and long-term coordination that makes a continuum of care successful. Finding sustainable funding for integrated care models can be a constant struggle.
Data interoperability sounds technical, but it has a very human impact. When different healthcare systems can’t easily share information, patients end up repeating their stories over and over, important details get lost, and care becomes fragmented instead of coordinated.
Staffing shortages affect many healthcare areas, especially in rural locations or specialized fields. When there aren’t enough qualified professionals available, it becomes much harder to provide consistent, high-quality care throughout the entire continuum.
Patient engagement can also be challenging. Some people may feel overwhelmed by their treatment plan or struggle to understand their role in the continuum of care, especially when they’re dealing with complex life circumstances.
Best Practices for a Successful Continuum of Care
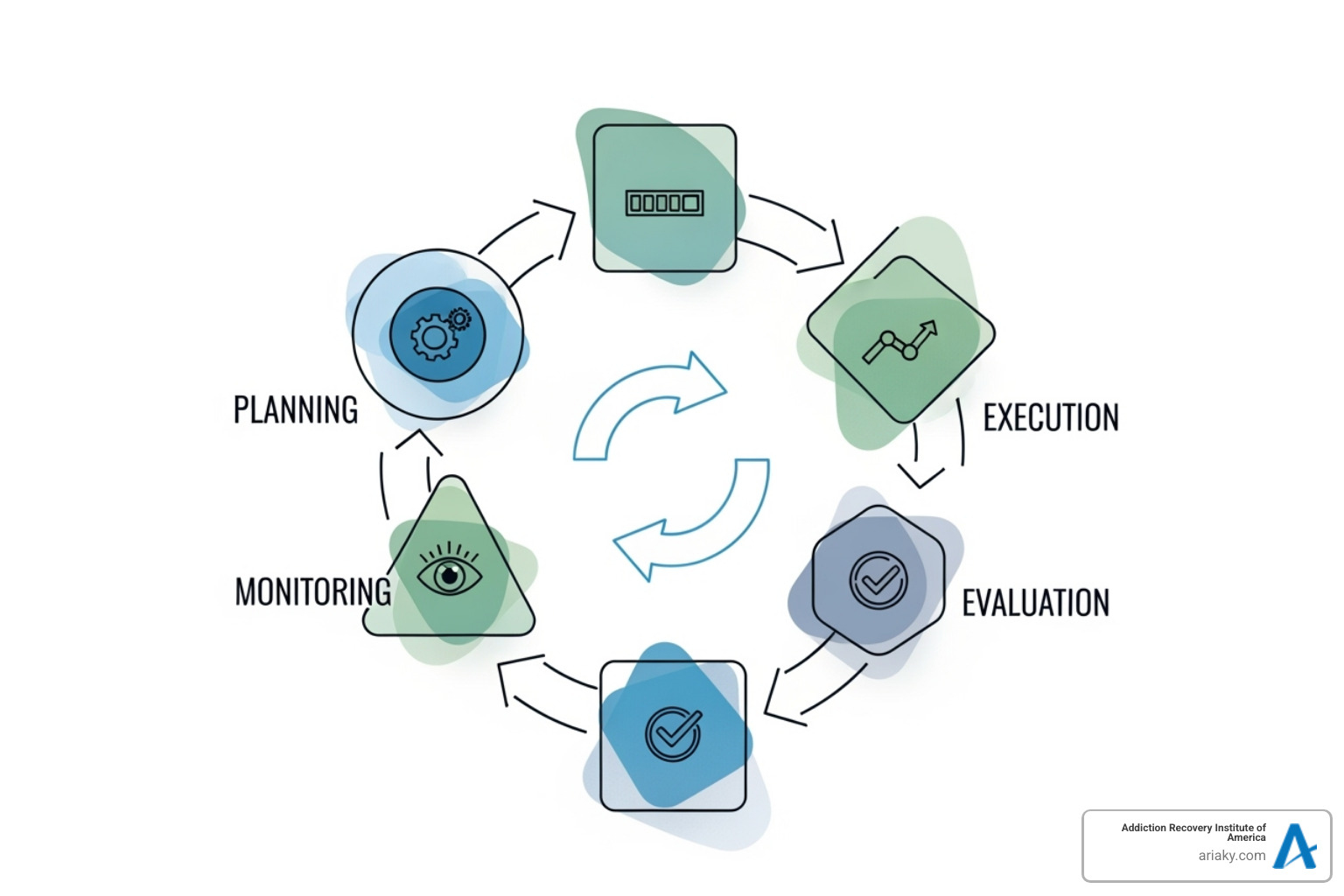
Despite these challenges, there are proven strategies for building and maintaining an effective continuum of care. The key is focusing on connection, communication, and continuous improvement.
Strengthening communication between all providers is absolutely essential. This means more than just sharing information – it requires active collaboration and regular discussions about patient needs and progress. When everyone is truly talking to each other, gaps in care become much less likely.
Standardizing records throughout the healthcare system creates a foundation for coordinated care. When every provider has access to complete, accurate patient information, they can make better decisions and avoid duplicating services. This also helps identify care gaps and track improvements over time.
Establishing clear success metrics helps everyone understand whether the continuum of care is actually working. By setting measurable goals and tracking outcomes, healthcare systems can continuously evaluate their effectiveness and make necessary improvements. This data-driven approach ensures that changes lead to better patient results.
Patient-centered care should be at the heart of every decision. This means involving patients and their families in treatment planning, respecting their preferences and goals, and tailoring care plans to meet individual needs. When people feel heard and involved in their own care, they’re more likely to stay engaged throughout their recovery journey.
Leveraging technology can help connect different services and improve efficiency. Electronic health records, telehealth services, and data analytics all play important roles in creating seamless transitions between different levels of care.
Fostering collaboration between healthcare organizations, social services, and community groups creates a broader support network for patients. These partnerships ensure that people have access to comprehensive support that addresses all aspects of their recovery.
The most successful continuum of care frameworks are those that remain flexible and responsive to changing needs. By continuously evaluating and adapting their approaches, healthcare systems can build robust support systems that truly serve individuals throughout their entire recovery journey.
Frequently Asked Questions about the Continuum of Care
We understand that the continuum of care can seem like a complex concept at first. That’s completely normal! Over the years, we’ve heard many thoughtful questions from individuals and families trying to understand how this approach can benefit their recovery journey. Let’s explore the most common questions together.
How does the continuum of care improve patient outcomes?
The continuum of care creates a powerful foundation for better health outcomes by weaving together all aspects of treatment into one cohesive support system. Think of it like having a dedicated team that never loses sight of your progress, no matter where you are in your recovery journey.
Coordinated care is perhaps the biggest game-changer. When your detox team communicates seamlessly with your residential counselors, who then work closely with your outpatient therapists, everyone stays on the same page about what’s working and what needs adjustment. This eliminates the confusion and gaps that often happen when providers work in isolation.
Reduced readmissions become a natural result of this coordinated approach. Because your care team plans thoroughly for each transition and provides robust follow-up support, you’re much better equipped to handle challenges that might otherwise lead to relapse or crisis situations.
Increased patient satisfaction flows naturally from feeling truly supported. A 2021 Journal of General Internal Medicine report found that patients receiving coordinated care reported significantly greater satisfaction with their treatment experience. When you know your entire care team is working together for your success, it creates a sense of security and confidence.
The long-term improvement statistics are particularly encouraging. Research shows that patients who follow a comprehensive continuum of care model demonstrate significantly greater levels of improvement over extended periods – sometimes maintaining progress for 10 years or more. This isn’t just about getting through treatment; it’s about building a foundation for lifelong wellness.
What is the difference between continuum of care and case management?
This question comes up frequently, and it’s easy to see why these concepts might seem similar at first glance. The key difference lies in scope and function.
The continuum of care represents the overall system or framework – imagine it as the entire highway system designed to get you from point A to point B safely and efficiently. It includes all the services, facilities, professionals, and protocols that work together to provide comprehensive care across different stages of treatment and recovery.
Case management, however, is a specific service within that larger system. Your case manager acts like a skilled navigator who knows the highway system inside and out. They focus on individual patient navigation, helping you understand your options, connecting you with appropriate resources, and advocating for your specific needs as you move through different levels of care.
So while the continuum of care provides the roadmap and infrastructure, case management offers the personalized guidance to help you steer that system successfully. Both are essential, but they serve different roles in supporting your recovery journey.
How is technology changing the continuum of care?
Technology is revolutionizing how we deliver and coordinate care, making the continuum of care more efficient, accessible, and personalized than ever before.
Electronic Health Records (EHRs) serve as the digital backbone of modern coordinated care. When these systems work together properly, your entire care team can access your complete treatment history, current medications, and progress notes in real-time. This means no more repeating your story to every new provider or worrying about important information getting lost between appointments.
Telehealth has opened up incredible possibilities for maintaining continuity of care. Whether you’re in a rural area with limited transportation or simply need flexible scheduling around work and family commitments, virtual sessions ensure your support continues uninterrupted. This technology has been particularly valuable for ongoing counseling and check-ins during outpatient phases of treatment.
AI-powered platforms are beginning to offer exciting new ways to personalize and improve care coordination. These systems can identify patterns in your progress, predict potential challenges, and suggest interventions before problems become crises. Some platforms now offer interactive assessments and automated check-in programs that provide continuous support between formal appointments.
Data analytics help treatment centers like ours continuously improve our continuum of care by analyzing outcomes across different treatment pathways. This data-driven approach allows us to refine our programs and identify the most effective combinations of services for different types of patients.
The result is a more connected, responsive, and effective treatment experience that adapts to your unique needs while maintaining the human touch that’s so crucial for recovery success.
Conclusion: Your Path to Seamless, Integrated Care
Throughout this journey, we’ve finded how the continuum of care serves as a lifeline for anyone seeking lasting health and recovery. From understanding its core components to seeing it in action across different healthcare settings, one thing becomes crystal clear: integrated, coordinated care isn’t just better care—it’s transformative care.
The beauty of a true continuum of care lies in its holistic approach. It doesn’t just address symptoms or isolated problems. Instead, it recognizes that healing happens over time, through different stages, with varying levels of support. Whether you’re dealing with addiction, managing a chronic condition, or supporting a loved one through their health journey, this comprehensive approach offers something invaluable: the assurance that you’re never alone.
We’ve seen how this model reduces hospital readmissions, improves patient satisfaction, and creates those crucial safety nets that prevent people from falling through the cracks. More importantly, we’ve learned that when healthcare providers work together—sharing information, coordinating treatments, and truly communicating—patients don’t just get better; they thrive.
At ARIA Kentucky, this philosophy isn’t just something we talk about—it’s woven into everything we do. Our continuum of care begins the moment you reach out for help and continues long after you’ve completed formal treatment. From medically supervised detox through residential care, from intensive outpatient programs to ongoing aftercare support, we’re committed to being your steady companion on the road to recovery.
Recovery isn’t a destination you reach and then forget about. It’s a lifelong journey that deserves lifelong support. That’s why our approach emphasizes not just getting sober, but building the skills, connections, and resilience needed for lasting wellness. Our accredited, AODE-certified programs across Kentucky—from Ashland to Louisville, Bowling Green to Lexington—are designed with this long-term vision in mind.
The path to recovery can feel overwhelming, especially when you’re not sure where to start. But here’s what we want you to know: you don’t have to figure it out alone. A comprehensive continuum of care means having a team of professionals who understand your journey, anticipate your needs, and adjust support as you grow stronger.
If you’re ready to experience what seamless, integrated care can do for your recovery, we’re here to help. Find a comprehensive continuum of care in Kentucky and find how our personalized approach can make all the difference. You can also explore our various Aria Rehab Locations to find the support that’s right where you need it.
Your journey toward healing starts with a single step. Let us help you take it—and every step that follows.