Understanding Opiates: The Foundation of America’s Addiction Crisis
Opiates are natural drugs from the opium poppy plant, used for centuries to treat pain but carrying high risks of addiction and overdose. Understanding what opiates are is crucial for making informed decisions about pain management, treatment, and recovery.
Quick Facts About Opiates:
- Natural Origin: Derived from the opium poppy plant
- Common Examples: Morphine, codeine, and opium
- Medical Uses: Pain relief, cough suppression, diarrhea treatment
- Addiction Risk: Highly addictive with potential for overdose
- Brain Impact: Bind to opioid receptors, releasing dopamine and blocking pain signals
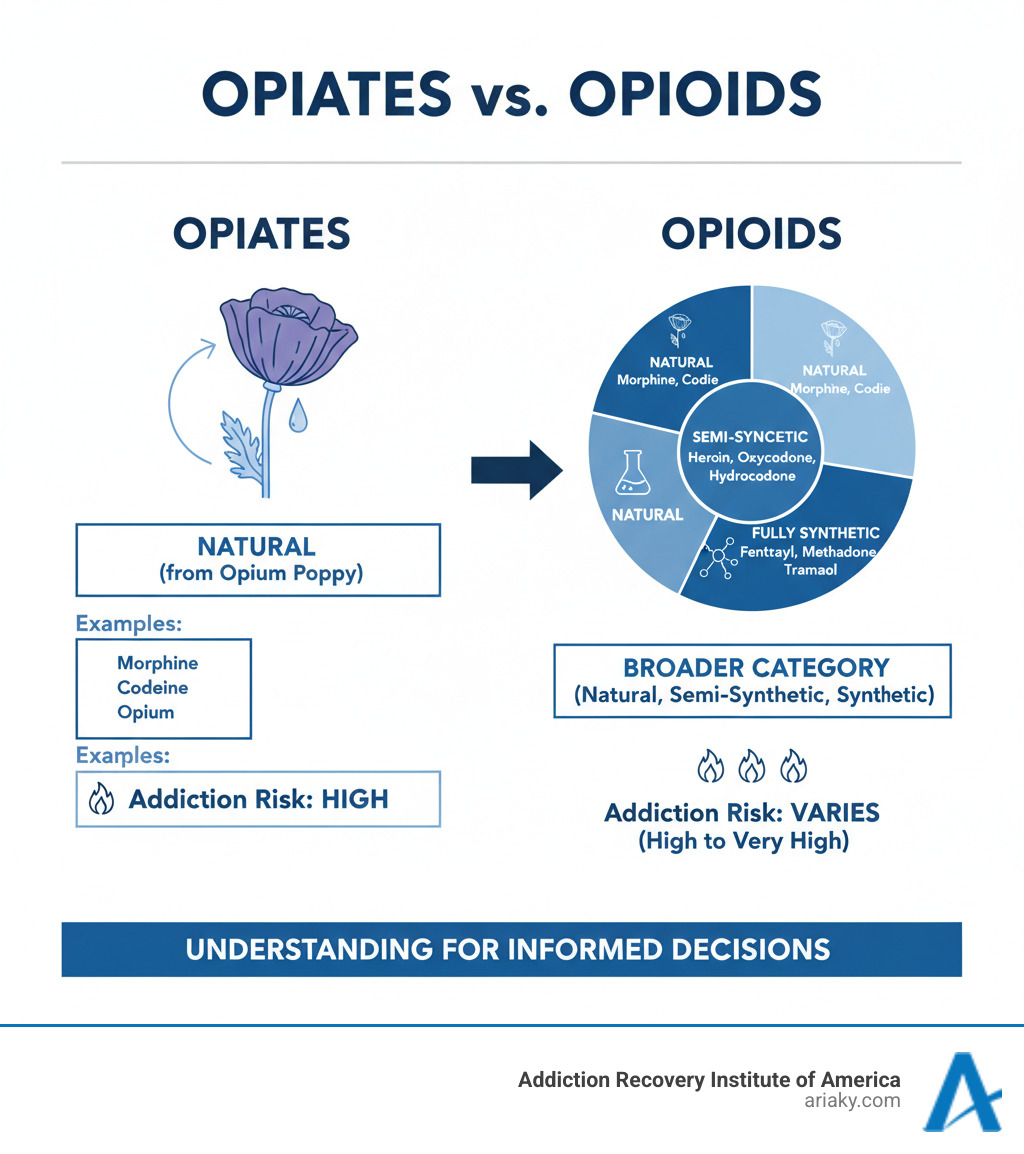
The terms “opiates” and “opioids” are often confused. Opiates are natural, while the broader category of opioids includes semi-synthetic (heroin, oxycodone) and fully synthetic versions (fentanyl).
This distinction is critical, as about 75% of people who became addicted to street opioids like heroin in the 2000s started with prescription medications. Understanding these substances is the first step toward safety and recovery. The good news is that opioid addiction is treatable. With medical supervision, medication, and therapy, lasting recovery is achievable.
Opiates vs. Opioids: The Definitive Guide
If you’ve ever been confused by the terms “opiates” and “opioids,” you’re not alone. The key difference is simple: opiates come straight from nature, while opioids include everything that works like opiates—whether natural, lab-modified, or completely man-made.
Opiates are the original pain relievers, extracted directly from the opium poppy plant. The three main natural opiates are opium, morphine, and codeine.

Opioids are the larger family. All opiates are opioids, but not all opioids are opiates. Scientists created two other categories:
Semi-synthetic opioids start as natural opiates but are chemically altered. Heroin, for example, is modified morphine. Prescription painkillers like oxycodone and hydrocodone are also in this group.
Fully synthetic opioids are created entirely in a lab to mimic the effects of opiates. Fentanyl, which is 50-100 times stronger than morphine, is a major driver of overdose deaths. Methadone, used in addiction treatment, is also synthetic.
| Category | Origin | Examples |
|---|---|---|
| Natural Opiates | Directly from opium poppy plant | Opium, Morphine, Codeine |
| Semi-Synthetic Opioids | Chemically modified natural opiates | Heroin, Oxycodone, Hydrocodone, Hydromorphone, Oxymorphone |
| Fully Synthetic Opioids | Entirely man-made in a laboratory | Fentanyl, Methadone, Tramadol, Buprenorphine |
Common Medical Uses for Opiates and Opioids
Despite their risks, opiates and opioids are vital medical tools when used correctly under supervision.
- Pain management: They are essential for severe pain from surgery, cancer, or major injuries.
- Anesthesia: Strong opioids help keep patients unconscious and comfortable during surgery.
- Cough suppression: Opiates like codeine are effective at quieting the cough reflex.
- Severe diarrhea: Opioids slow the digestive system. Loperamide (Imodium) is an opioid that doesn’t affect the brain.
- Opioid addiction treatment: Medications like methadone and buprenorphine are used to help people break the cycle of street drug use and stabilize their lives.
The Evolution of Terminology
The term “opiate” came first, referring to drugs from the poppy plant. As scientists created synthetic versions, the broader term “opioid” was needed to cover all substances that bind to opioid receptors. Today, health organizations like the CDC primarily use “opioid” to describe the full scope of the crisis. The term “narcotic” is an older, less precise term often used in legal contexts.
The Science Behind Opiates: How They Impact Your Brain and Body
Opiates work by hijacking the body’s natural pain relief system. Your brain produces its own painkillers called endorphins. Opiates and opioids mimic these chemicals, binding to opioid receptors in your brain, spine, and gut.
When an opiate molecule locks into a receptor, it blocks pain signals. It also triggers a massive release of dopamine, the brain’s pleasure chemical, creating intense euphoria. This dopamine surge is what makes these drugs so addictive.
As central nervous system depressants, opiates slow down vital functions. Short-term effects include:
- Drowsiness or “nodding off”
- Confusion
- Nausea and vomiting
- Constipation
- Slowed breathing (respiratory depression), which is the most dangerous effect and can lead to a fatal overdose.
Long-term opiate use changes the brain’s structure, leading to tolerance, dependence, and addiction. It can also disrupt hormone levels and, paradoxically, increase pain sensitivity over time (hyperalgesia).
Tolerance, Dependence, and Addiction Explained
These terms describe different stages of opioid use:
- Opioid tolerance is when you need a higher dose to get the same effect. Your body has adapted to the drug.
- Physical dependence means your body has adjusted to the drug’s presence and will experience withdrawal symptoms if you stop. This is a normal physiological response and can happen even when taking medication as prescribed.
- Opioid Use Disorder, or addiction, is a brain disease characterized by compulsive drug use despite negative consequences. It involves changes to brain circuits related to reward, motivation, and memory.
Opioid Withdrawal Symptoms
When a physically dependent person stops using opiates, they experience withdrawal. Symptoms usually start within 4-12 hours, peak in 1-3 days, and can last for about a week, though some psychological symptoms linger.
Common symptoms include:
- Intense drug cravings
- Muscle aches and bone pain
- Nausea, vomiting, and diarrhea
- Anxiety and agitation
- Insomnia
- Cold flashes with goosebumps (the origin of “going cold turkey”)
- Sweating, runny nose, and watery eyes
Withdrawal is uncomfortable and is a major barrier to quitting without medical help. Medically supervised detox can manage these symptoms, making recovery safer and more achievable.
Recognizing the Risks: From Misuse to Overdose
The path from legitimate pain management to addiction often starts innocently. Prescription opioid misuse can include taking more than prescribed, using someone else’s medication, or continuing use after the pain has subsided.
This progression is a common gateway to illicit drug use. Statistics show that about 75% of people in the U.S. who became addicted to street opioids such as heroin during the 2000s report that they started out taking prescription opioid drugs. As tolerance builds, prescription drugs become expensive and hard to get, making cheaper, more available street drugs like heroin an alternative.
The most immediate risk of any opioid use is overdose. Opioids can cause respiratory depression, where breathing slows down or stops completely. This leads to hypoxia (oxygen deprivation), which can cause permanent brain damage or death within minutes.

Fortunately, an opioid overdose can often be reversed with naloxone (Narcan), a medication that blocks opioid receptors. Having naloxone available can save a life.
Signs and Symptoms of Opioid Use Disorder
Recognizing Opioid Use Disorder (OUD) can be difficult. Look for a pattern of these signs:
- Behavioral Changes: Withdrawing from friends and family, neglecting work or home responsibilities, financial problems, or “doctor shopping” for more prescriptions.
- Physical Signs: Pinpoint pupils, unexplained weight loss, constant drowsiness or “nodding off,” and slurred speech.
- Psychological Signs: Severe mood swings, confusion, memory problems, and an obsession with obtaining and using the drug.
If you see these signs, it’s time to seek professional help. OUD is a treatable medical condition.
The Dangers of Mixing Opiates with Other Substances
Combining opiates with other substances dramatically increases overdose risk.
- Alcohol and Benzodiazepines (e.g., Xanax, Valium): Both are depressants that, when mixed with opioids, can multiply the effect on breathing, leading to fatal respiratory arrest.
- Stimulants (e.g., cocaine, methamphetamine): These can mask the sedative effects of opiates, causing a person to take a dangerously high dose. When the stimulant wears off, the full opioid dose hits at once, often causing an overdose.
Never combine opiates with other substances unless directed by a doctor who is aware of all your medications.
Opioid Use During Pregnancy
Opiate use during pregnancy poses serious risks to both mother and baby. Mothers face a higher risk of complications, while babies can be born with Neonatal Abstinence Syndrome (NAS), a painful and dangerous withdrawal condition. Other risks for the baby include low birth weight and premature birth.
Quitting opioids suddenly during pregnancy is also dangerous. The safest approach is Medication-Assisted Treatment (MAT) with methadone or buprenorphine under a doctor’s care. This stabilizes both mother and baby and greatly improves outcomes. Pregnant women struggling with opiate use should seek immediate, non-judgmental medical help.
The Path to Recovery: Treatment for Opioid Use Disorder
Recovery from opiates and opioid addiction is possible. At ARIA Kentucky, we know that while addiction is a chronic disease, it responds well to a combination of medical care and support.
Medication-Assisted Treatment (MAT) is the gold standard for treating opioid use disorder (OUD). It combines FDA-approved medications with counseling to address both the physical and psychological aspects of addiction.
- Buprenorphine (Suboxone) is a partial opioid agonist that reduces cravings and withdrawal without producing a high. It can be prescribed in an office setting.
- Methadone is a full opioid agonist that eliminates withdrawal and cravings. It is dispensed at specialized clinics, providing structure and stability.
- Naltrexone (Vivitrol) is an opioid blocker. It prevents a person from feeling the effects of opioids, which can help prevent relapse after detox.
Behavioral therapies are a critical part of recovery. Cognitive Behavioral Therapy (CBT) helps change destructive thought patterns, while group and individual therapy provide support and address the root causes of addiction.
Detoxification is the first step, managing withdrawal symptoms to prepare a person for treatment. It is not a cure on its own. Treatment can occur in an inpatient (residential) setting for 24/7 support or through outpatient programs (PHP/IOP) that allow for more flexibility.
What is Naloxone and How Does it Work?
Naloxone is a life-saving medication that can reverse an opiate overdose. It works as an opioid antagonist, knocking opioid molecules off brain receptors and restoring normal breathing within minutes.
Naloxone is available as a simple-to-use nasal spray (Narcan) or an injection. If you suspect an overdose (unresponsive, slow or no breathing, blue lips/fingernails):
- Call 911 immediately. Medical attention is essential, even if naloxone is used.
- Administer naloxone according to the package directions. Give a second dose if there’s no response in 2-3 minutes.
- Stay with the person and try to keep them breathing. Place them on their side to prevent choking.
Naloxone is safe and has no effect on someone who has not taken opioids. Knowing how to use it can save a life.
Frequently Asked Questions about Opiates
We receive many questions about opiates and opioids. Here are answers to some of the most common concerns.
Can eating poppy seeds make you fail a drug test?
Yes, it’s possible. Poppy seeds can be contaminated with trace amounts of morphine and codeine during harvesting. While most modern drug tests use a high threshold (around 2000 ng/mL) to distinguish food consumption from drug use, eating a large quantity of poppy seeds could potentially trigger a positive result. To be safe, it’s best to avoid poppy seeds for a few days before a scheduled drug test.
Who is most at risk for opioid addiction?
Addiction can affect anyone, but some factors increase the risk:
- Age: Younger adults (under 29) have the highest rates of opiate use.
- Gender: Men are twice as likely as women to develop an opiate addiction.
- Personal History: A prior history of substance abuse or mental health conditions like depression, anxiety, or PTSD significantly increases risk.
- First Exposure: 75% of people who became addicted to street opioids like heroin started with prescription medications.
- Environment: Factors like poverty, unemployment, trauma, and growing up around substance use also contribute to risk.
What are the legal and societal impacts of opioid misuse?
The opiate crisis has had a devastating impact on society.
- Legal System: Jails and prisons are overwhelmed with individuals arrested for drug-related offenses. Police resources are strained.
- Healthcare: Emergency rooms are flooded with overdose cases, and the cost of long-term treatment and related health issues (HIV, hepatitis) is astronomical.
- Families and Communities: The crisis fuels the foster care system, burdens families, increases crime, and lowers property values.
- Economy: Lost productivity from unemployment and on-the-job impairment, combined with rising healthcare premiums, damages the economy.
- Public Health: Overdose deaths have lowered the average life expectancy in the U.S. The stigma surrounding addiction often prevents people from seeking the help they need.
The crisis has forced a shift from punishment toward a public health approach focused on treatment, prevention, and compassion.
Conclusion
We’ve covered the critical differences between opiates (natural) and the broader category of opioids (including synthetics). This knowledge is vital, as all these substances hijack the brain’s reward system and can lead from tolerance to dependence and addiction.
The statistic that 75% of people who became addicted to heroin started with prescription opioids highlights how easily this can happen. The risks are real, but so is the hope for recovery.
Addiction is a treatable disease. With the right help, the brain can heal. Medication-Assisted Treatment (MAT), combined with counseling, gives people their lives back. We see it happen every day.
If you or a loved one is struggling, you are not alone. Recovery is more than possible—it can be the start of a new, better chapter.
At ARIA Kentucky, our AODE-certified team creates individualized treatment plans, from detox to outpatient care, to meet you where you are. Your story doesn’t have to end with addiction.
Learn more about our comprehensive heroin detox programs and take the first step towards recovery: Heroin Detox at ARIA Kentucky

