What Is Delirium Tremens and Why Should You Care?
Delirium tremens (DTs) is the most severe form of alcohol withdrawal, a life-threatening emergency that occurs when a heavy drinker suddenly stops. It affects about 3-5% of people in alcohol withdrawal and is fatal in 5-15% of cases, even with medical treatment.
Quick Facts About Delirium Tremens:
- What it is: Severe alcohol withdrawal with confusion, tremors, and hallucinations
- When it happens: Usually 48-96 hours after the last drink (can be up to 10 days)
- Who’s at risk: People with chronic heavy drinking, especially those who’ve had withdrawal seizures before
- Key symptoms: High fever, rapid heart rate, severe confusion, vivid hallucinations, tremors
- Mortality rate: 5-15% with treatment, up to 40% without medical care
- Treatment: Requires immediate hospitalization and intensive medical care
If you or someone you know has alcohol withdrawal symptoms, do not handle it alone. Delirium tremens is a medical emergency requiring immediate professional intervention.
The name comes from Latin for “trembling delirium.” When alcohol is suddenly removed, the brain, which has adapted to its presence, goes into a state of overdrive.
While about 29% of U.S. adults will face alcohol use disorder, only a small fraction of those in withdrawal develop DTs. For those who do, it can be deadly without medical care.
The good news is that with hospital treatment, most people survive delirium tremens and can achieve lasting recovery from alcohol addiction.
What Causes Delirium Tremens and Who Is at Risk?
Chronic heavy drinking alters brain chemistry. Alcohol improves the calming neurotransmitter GABA and suppresses the excitatory one, glutamate. To compensate, the brain increases its excitatory activity. When alcohol is suddenly withdrawn, this system becomes dangerously overexcited, triggering the hyperexcitability of delirium tremens.
This rewiring of the central nervous system becomes more dramatic with longer and heavier drinking. When alcohol is removed, the brain swings wildly in the opposite direction, creating the dangerous symptoms of DTs.
Who’s Most at Risk?
Only about 3-5% of people in alcohol withdrawal develop delirium tremens, but certain factors dramatically increase the risk:
- Heavy, long-term drinking: Years of heavy drinking give the brain time to develop these dangerous adaptations.
- Previous withdrawal seizures: A history of severe withdrawal primes the brain for worse reactions, a process known as “kindling.”
- Age over 30: DTs are most common in this age group, likely due to cumulative damage and other health issues.
- Co-occurring medical problems: Malnutrition, liver disease, heart problems, or infections increase the risk.
- Abrupt cessation: Suddenly stopping alcohol causes the most dramatic brain chemistry shifts.
- Other substance use: Using other depressants like benzodiazepines can compound withdrawal effects.
Research also shows that high education, low obesity, and reduced alcohol intake correlated with a lower risk of delirium, highlighting the role of overall health.
If you have a history of heavy drinking and want to quit, do not do it alone. The risks are too high, and medically supervised detox can save your life.
Recognizing the Symptoms and Diagnosing DTs
Delirium tremens is a medical crisis with distinct, severe symptoms. Recognizing them can save a life.

Key symptoms of the nervous system in overdrive include:
- Autonomic hyperactivity: A racing heart (tachycardia), high blood pressure, fever, and profuse sweating.
- Global confusion: Severe disorientation about time, place, or identity.
- Severe agitation: Extreme restlessness, sometimes leading to combativeness.
- Hallucinations: Vivid and terrifying visual, auditory, or tactile experiences, such as seeing insects on the skin (formication).
- Tremors: Severe, uncontrollable, whole-body trembling.
- Seizures: Also known as “rum fits,” these can occur without warning.
- Sleep disturbances: Intense insomnia followed by periods of deep, prolonged sleep.
Diagnosing delirium tremens requires a skilled medical team. Diagnosis involves a physical exam, a patient history of alcohol use, and standardized tools like the Clinical Institute Withdrawal Assessment for Alcohol (CIWA-Ar) scale to measure symptom severity. A score over 15 often indicates a high risk for DTs. Blood and urine tests are used to check organ function, rule out other conditions, and identify electrolyte imbalances. For detailed clinical guidance, providers can consult resources like Recognition and management of withdrawal delirium (delirium tremens).
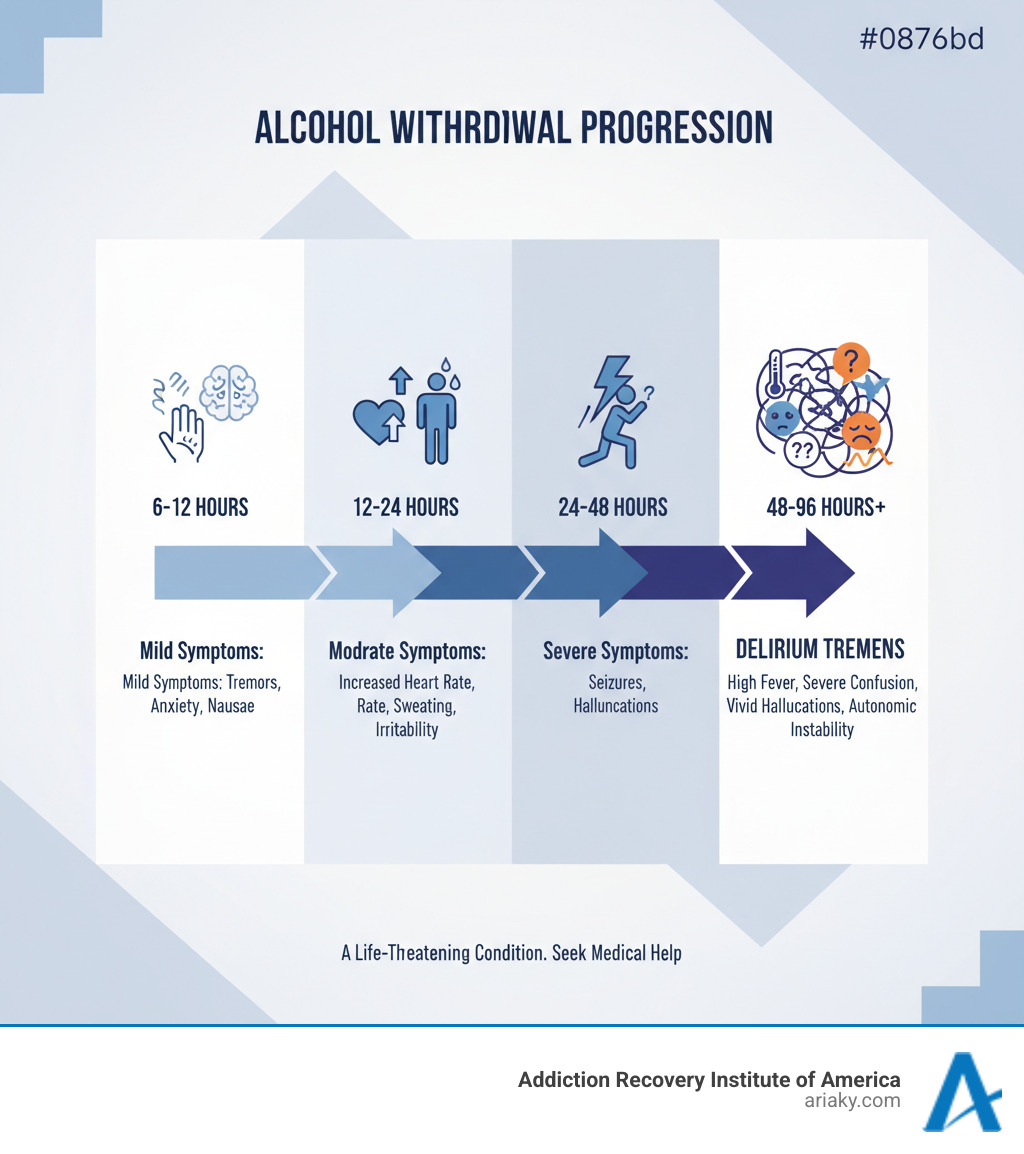
The Timeline of Alcohol Withdrawal and Delirium Tremens Symptoms
DTs is the final stage of a progressive withdrawal process:
- Early withdrawal (6-12 hours): Minor symptoms like anxiety, tremors, headaches, and nausea.
- Peak withdrawal (12-48 hours): Symptoms intensify. Heart rate and blood pressure climb. Alcoholic hallucinosis (where the person knows the hallucinations aren’t real) and withdrawal seizures are most common in this phase.
- Late withdrawal (48-96 hours): Delirium tremens typically appears. This is when severe confusion, high fever, and terrifyingly real hallucinations emerge. While this is the typical window, DTs can be delayed for up to 10 days.
Differentiating DTs from Other Conditions
Medical expertise is crucial because DTs can mimic other serious conditions:
- Wernicke encephalopathy: A brain disorder from thiamine (Vitamin B1) deficiency, causing confusion and coordination loss.
- Hepatic encephalopathy: Occurs when a damaged liver can’t filter toxins, leading to confusion and tremors.
- Other causes: Sepsis (severe infection), head injuries, and metabolic problems can also cause delirium.
Comprehensive testing is necessary to ensure an accurate diagnosis, as each condition requires a different life-saving treatment.
How Is Delirium Tremens Treated?
Delirium tremens is a medical emergency requiring immediate hospitalization, often in an Intensive Care Unit (ICU). With prompt medical care, most people recover.

Treatment priorities include:
- Continuous monitoring: Around-the-clock observation of heart rate, blood pressure, temperature, and breathing.
- Supportive care: Creating a calm, quiet, well-lit environment to reduce agitation and confusion.
- Hydration and nutrition: IV fluids are used to correct dehydration and replace essential minerals like magnesium and phosphate.
- Thiamine supplementation: High-dose IV thiamine is crucial to prevent Wernicke encephalopathy, a form of brain damage. It must be given before any glucose.
Treatment is often guided by symptom-triggered therapy, where medication doses are adjusted based on symptom severity, measured by tools like the CIWA-Ar scale. This personalized approach helps control symptoms without over-sedation. For more on emergency management, providers can see Management of Alcohol Withdrawal in the Emergency Department: Current Perspectives.
The Role of Benzodiazepines in Treating Delirium Tremens
Benzodiazepines are the cornerstone of DTs treatment. They work by enhancing the brain’s calming GABA neurotransmitter, substituting for alcohol’s effect and reducing the dangerous hyperexcitability.
- Diazepam (Valium) is a fast-acting, long-lasting option.
- Lorazepam (Ativan) is preferred for patients with liver problems.
- Chlordiazepoxide (Librium) is another long-acting choice.
Dosing is custom to the patient’s symptoms. While effective, benzodiazepines require careful monitoring. Researchers are exploring other options, such as those in Valproate-Improved Protocols for Alcohol Withdrawal Syndrome, to improve outcomes.
Adjunctive and Refractory Treatment Options
When high doses of benzodiazepines are not enough (refractory DTs), other medications are used in an ICU setting:
- Phenobarbital: This barbiturate also improves the GABA system and can reduce the need for mechanical ventilation, as shown in studies on its use with benzodiazepines and in alcohol withdrawal syndrome.
- Dexmedetomidine (Precedex): Provides sedation without suppressing breathing, a major advantage in the ICU.
- Propofol (Diprivan): A potent anesthetic for the most severe, treatment-resistant cases, requiring intensive monitoring.
- Ketamine: An emerging option for cases that resist conventional therapy.
Antipsychotics like haloperidol may be used for severe hallucinations but require caution as they can lower the seizure threshold. The goal is to safely calm the brain’s hyperexcitability, allowing it to restore its chemical balance.
Complications, Prognosis, and Long-Term Outlook
Delirium tremens is a medical emergency with serious, life-threatening complications. Even with modern medical care, the mortality rate is 5-15%. Without treatment, it jumps to a frightening 15-40%. The most common causes of death are respiratory failure and cardiac arrhythmias due to the incredible stress on the body.
Beyond the risk of death, potential complications include:
- Seizures: Can lead to serious injury or choking.
- Aspiration pneumonia: A dangerous lung infection caused by inhaling stomach contents.
- Rhabdomyolysis: Severe muscle breakdown that can cause kidney failure.
- Wernicke-Korsakoff syndrome: Permanent brain damage from thiamine deficiency, affecting memory and cognition.
Even after recovery, some people experience lingering issues with memory or concentration. Outcomes can be varied, as detailed in research like Varied Outcomes of Prolonged Delirium Tremens – A Case Series.
Prognosis and Prevention
The good news is that with prompt medical care, survival rates for delirium tremens can exceed 95%. Early intervention saves lives. The outcome depends on symptom severity, other health problems, and how quickly a person gets to a hospital.
Prevention is always the best approach. For someone with an alcohol problem, the safest way to quit is through medically supervised detox. Never try to quit “cold turkey” if you’re a heavy drinker, as the abrupt stop is what triggers DTs. For many, lifelong abstinence is the surest way to prevent a recurrence.
Long-Term Management After Experiencing Delirium Tremens
Surviving delirium tremens is the first step. The real work begins with addressing the underlying alcohol use disorder. Comprehensive addiction treatment is essential for lasting recovery.
Treatment options often begin with a Detox Program and may include:
- Inpatient rehabilitation: A structured environment focused on recovery.
- Outpatient programs: Our Partial Hospitalization (PHP) and Intensive Outpatient (IOP) programs offer intensive treatment while allowing clients to live at home.
- Counseling and therapy: Individual and group therapy, especially Cognitive Behavioral Therapy (CBT), helps develop coping skills and change thought patterns.
- Support groups: Peer support from groups like Alcoholics Anonymous and SMART Recovery is invaluable.
Treating co-occurring mental health issues like depression or anxiety is also critical. Lifestyle changes, family support, and ongoing medical care are all key components of a strong recovery foundation. The National Institute on Alcohol Abuse and Alcoholism offers excellent resources on alcohol’s health effects.
At ARIA Kentucky, our Addiction Treatment and Alcohol Abuse Treatment programs are custom to each person’s needs. We’ve helped many people move from the crisis of delirium tremens to building meaningful, sober lives. To learn more, visit our Blog.
You don’t have to do this alone. Help is available, and recovery is possible.
Frequently Asked Questions about Delirium Tremens
Here are answers to common questions about delirium tremens.
How long does delirium tremens last?
Delirium tremens typically lasts 3 to 7 days, with symptoms peaking around day four or five. The exact duration depends on a person’s drinking history, overall health, and how quickly they receive medical treatment. Complications like infections can extend the recovery period. Even after the acute phase, some effects like anxiety or difficulty concentrating can linger for weeks or months as the brain heals.
Can you die from delirium tremens?
Yes, delirium tremens is a deadly medical emergency. Without treatment, the mortality rate is 15% to 40%. With proper hospital care, the rate drops to 5% to 15%, meaning 85% to 95% of people survive. The most common causes of death are respiratory failure, life-threatening cardiac arrhythmias, and severe electrolyte imbalances. Prompt medical attention is critical for survival.
What are the “pink elephants” associated with delirium tremens?
“Pink elephants” is a cultural shorthand for the vivid and frightening visual hallucinations that can occur during delirium tremens. While the content varies, these experiences feel completely real and cause intense fear and agitation. A common tactile hallucination is formication, the sensation of insects crawling on the skin. These are symptoms of a medical condition, not a personal failing, and understanding this helps family members provide support.
Conclusion
The most important takeaway is that delirium tremens is a serious medical emergency requiring immediate professional help. It should never be handled at home. The symptoms are not a sign of weakness but a physiological cry for help from a brain in overdrive after the sudden cessation of heavy, long-term alcohol use.
Seeking medical help is life-saving, dramatically reducing the mortality rate. Surviving delirium tremens can be a powerful catalyst for change, motivating individuals to pursue lasting recovery from alcohol use disorder.
The journey to sobriety involves comprehensive care, including therapy, support groups, and lifestyle changes. It’s a challenging but rewarding path to a healthier, clear-headed life.
At Addiction Recovery Institute of America (ARIA Kentucky), our team understands that behind every case of delirium tremens is a person who deserves compassionate, expert care. We have walked this path with countless individuals, helping them move from crisis to a hopeful future.
If you are ready to take the first step, we are here to help. Whether you need immediate assistance with alcohol withdrawal or are seeking comprehensive addiction treatment, our doors are open. Recovery is possible, and you don’t have to do it alone.


