Understanding Your Coverage: The First Step to Affordable Care
Does your insurance cover a partial hospitalization program? In most cases, yes—federal law requires most health insurance plans to cover mental health and substance use disorder treatment, including Partial Hospitalization Programs (PHPs). However, the specific coverage details depend on your individual plan, medical necessity, and whether you choose an in-network provider.
Quick Answer: Key Coverage Requirements
- Federal Mandate: The Affordable Care Act (ACA) and Mental Health Parity and Addiction Equity Act (MHPAEA) require most insurance plans to cover PHPs as essential health benefits
- Medical Necessity: Coverage requires a physician’s certification that you need intensive treatment to avoid inpatient hospitalization
- Plan Variables: Your deductible, copayment, coinsurance, and network status affect your out-of-pocket costs
- Medicare: Covers PHP when the doctor and program accept assignment
- Medicaid: Coverage varies by state but generally includes PHP services when medically necessary
- TRICARE: Provides coverage for PHP treatment for service members and veterans
- VA Health Care: Covers drug and alcohol use and mental health treatment for veterans
Struggling with substance use is overwhelming, and worrying about paying for treatment can make it harder. Many people delay getting help, unsure if their insurance will cover it.
The good news is that federal laws now require most insurance plans to cover addiction treatment, including PHPs. However, “covered” doesn’t mean “free,” and the details are important.
This guide will explain how insurance coverage works for PHPs, what questions to ask, how to verify benefits, and what to do about unexpected costs. By the end, you’ll be equipped to steer the insurance system and focus on what really matters—your recovery.
Easy does your insurance cover a partial hospitalization program glossary:
Navigating Your Path to Recovery: An Introduction to PHP
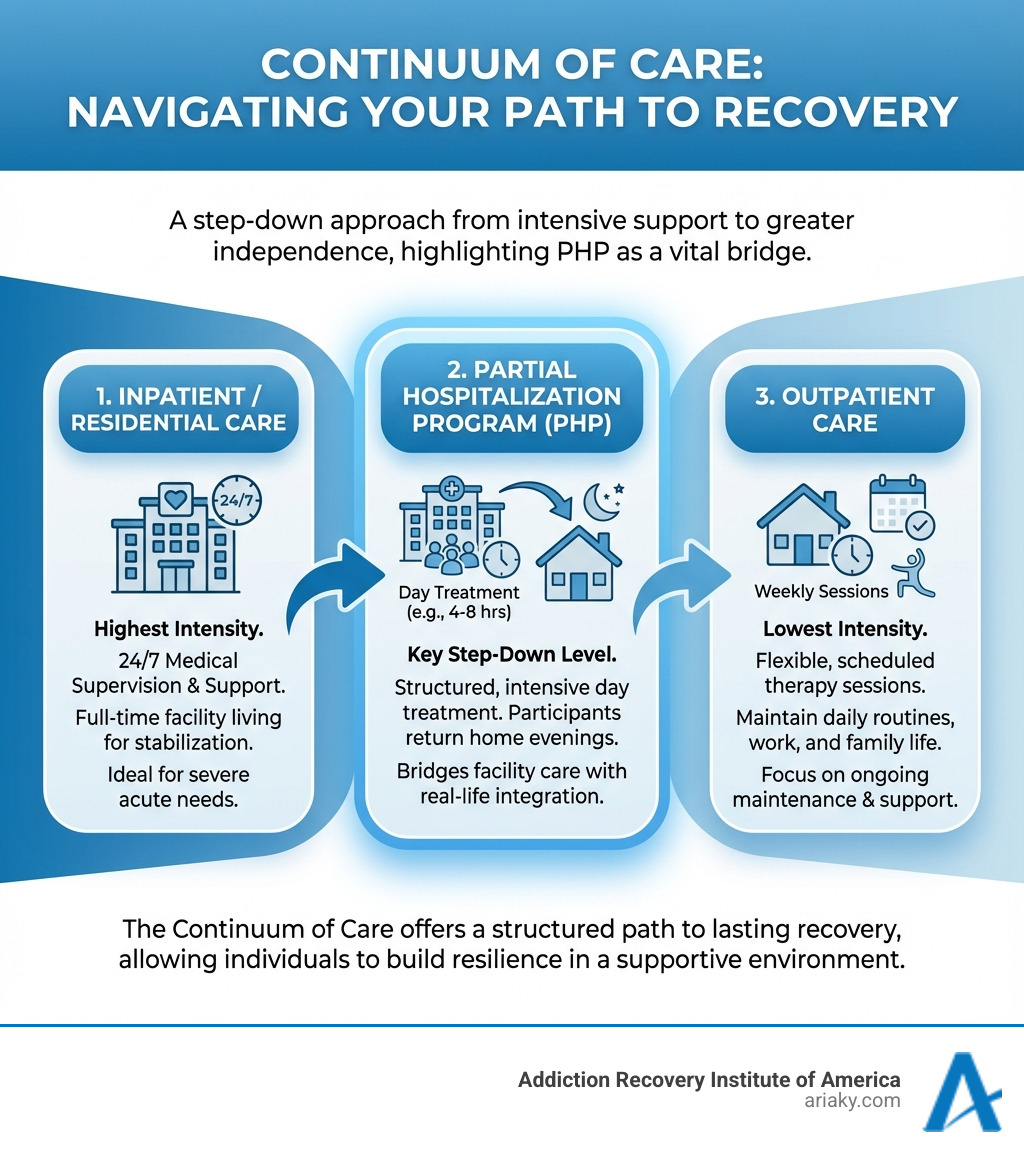
When navigating the complexities of mental health and addiction treatment, understanding the various levels of care available is crucial. Among these, the Partial Hospitalization Program (PHP) stands out as a vital bridge, offering intensive support without requiring an overnight stay. This unique structure allows individuals to receive comprehensive care while maintaining important connections to their home life and responsibilities.

What is a Partial Hospitalization Program (PHP)?
A Partial Hospitalization Program (PHP) is a highly structured, intensive outpatient treatment option for individuals who need significant support for mental health or substance use disorders but do not require 24-hour supervision. As a robust day treatment program, participants typically spend 4 to 8 hours a day at a facility, five days a week, before returning home in the evenings.
According to the Substance Abuse and Mental Health Services Administration (SAMHSA), Level 2 programs like PHPs focus on teaching coping strategies, relapse management, and providing psychosocial support. Our PHPs at Addiction Recovery Institute of America are designed to help individuals achieve these goals in a supportive environment, building resilience for lasting recovery.
PHPs are particularly effective for individuals with co-occurring disorders (a mental health condition and a substance use disorder). These programs provide integrated treatment that addresses both issues simultaneously for effective recovery.
The Key Differences: PHP vs. Inpatient and Outpatient Care
To appreciate the value of a PHP, it helps to understand its place within the broader continuum of care for mental health and addiction treatment.
| Feature | Inpatient/Residential Care | Partial Hospitalization Program (PHP) | Standard Outpatient Care |
|---|---|---|---|
| Intensity | Highest level; 24/7 medical supervision and support. | High level; structured, intensive day treatment. | Lowest level; flexible, weekly sessions. |
| Time Commitment | Full-time; live at the facility for weeks or months. | Part-time; 4-8 hours/day, 5 days/week; return home. | Minimal; typically 1-3 hours/week or a few times/week. |
| Living Situation | Reside at the treatment facility. | Live at home or in a supportive sober living environment. | Live at home; maintain daily routines. |
| Ideal Candidate | Severe addiction/mental illness, unstable, high risk, needs detox or stabilization. | Stepping down from inpatient, needing more support than outpatient, stable home environment. | Mild to moderate issues, stable, aftercare, strong support system. |
Inpatient care (residential treatment) is the most intensive level, providing 24/7 medical monitoring and therapy at a live-in facility. It’s ideal for severe cases, mental health crises, or medically supervised detox. Learn more in our Residential Treatment Kentucky Ultimate Guide.
Standard outpatient care is the least intensive, with weekly therapy sessions that allow individuals to maintain their daily routines. It’s suitable for mild conditions or as a step-down from more intensive programs. You can learn more about What is Outpatient Addiction Treatment?
A PHP is a crucial middle ground, offering the intensive structure of inpatient care during the day with the flexibility of returning home at night. This allows individuals to practice new skills in their real-world environment, making it an invaluable part of the recovery journey.
What are the Benefits of a PHP?
Choosing a PHP offers a unique blend of benefits for individuals seeking recovery from addiction or managing mental health challenges.
A primary benefit is the high level of care combined with flexibility. PHPs offer intensive, evidence-based therapies and medical supervision similar to inpatient care, but without an overnight stay. This allows individuals to receive robust treatment while maintaining family, work, or school commitments, making it ideal for those who cannot put their lives on hold.
PHPs also excel as transitional support. They provide a structured step-down from inpatient care, helping individuals reintegrate into daily life. For those needing more than standard outpatient care but not 24/7 supervision, a PHP offers the right level of intensive intervention, preventing relapse during a critical recovery phase.
Another advantage is the focus on developing real-world coping skills and fostering independence. Participants learn and practice coping mechanisms and relapse prevention strategies during the day, then apply them at home in the evenings. This immediate application builds confidence in managing daily triggers and stressors.
Finally, PHPs offer robust peer support and community building. Through group therapy programs and shared experiences, participants build a supportive network, reducing isolation and providing encouragement. Studies show that 92% of people in acute partial hospitalization programs improved, demonstrating the effectiveness of these structured environments.
So, Does Your Insurance Cover a Partial Hospitalization Program?
The short answer is yes, most insurance plans do cover a partial hospitalization program. However, the extent of coverage and your out-of-pocket costs depend on several key factors. Understanding these is essential for navigating the financial side of your recovery.
How Federal Laws Mandate PHP Coverage
The landscape of mental health and substance use disorder coverage has significantly improved due to key federal legislation.
The Affordable Care Act (ACA) of 2010 was pivotal. It requires health insurance providers to cover mental health and substance use disorders as essential health benefits, which includes PHPs. This means plans on the HealthCare.gov Marketplace cannot place a cap on this coverage (except for some older “grandfathered plans”).
The Mental Health Parity and Addiction Equity Act (MHPAEA) of 2008 is also crucial. It ensures that benefits for mental health and substance use disorders are no more restrictive than those for medical/surgical care. This “parity” applies to financial requirements (deductibles, copayments) and treatment limits (visit caps). Because of MHPAEA, most plans must offer some coverage for partial hospitalization.
These laws mean that most private insurance companies (like Blue Cross Blue Shield, Aetna Insurance, and Cigna) offer coverage for addiction recovery. However, specifics can still vary significantly regarding deductibles, copayments, and the distinction between in-network and out-of-network providers.
The Role of Medical Necessity in Getting Approved
Even with federal mandates, insurance companies require proof of “medical necessity” to cover PHP services. This means a qualified healthcare professional must certify that this level of care is clinically appropriate and necessary for your condition.
Insurance providers typically use established criteria, such as the American Society of Addiction Medicine (ASAM) criteria, to assess medical necessity. These criteria help determine the most appropriate level of care based on the severity of your symptoms, your ability to function, and any potential risks.
For a PHP to be deemed medically necessary, a physician or other qualified mental health professional must certify that you require intensive treatment and that without it, you would likely need inpatient psychiatric hospitalization. This justification ensures that the intensive resources of a PHP are used for those who truly need it.
Our treatment teams at Addiction Recovery Institute of America are experts in conducting clinical assessments and working with insurance providers to ensure that the medical necessity for your PHP is clearly documented.
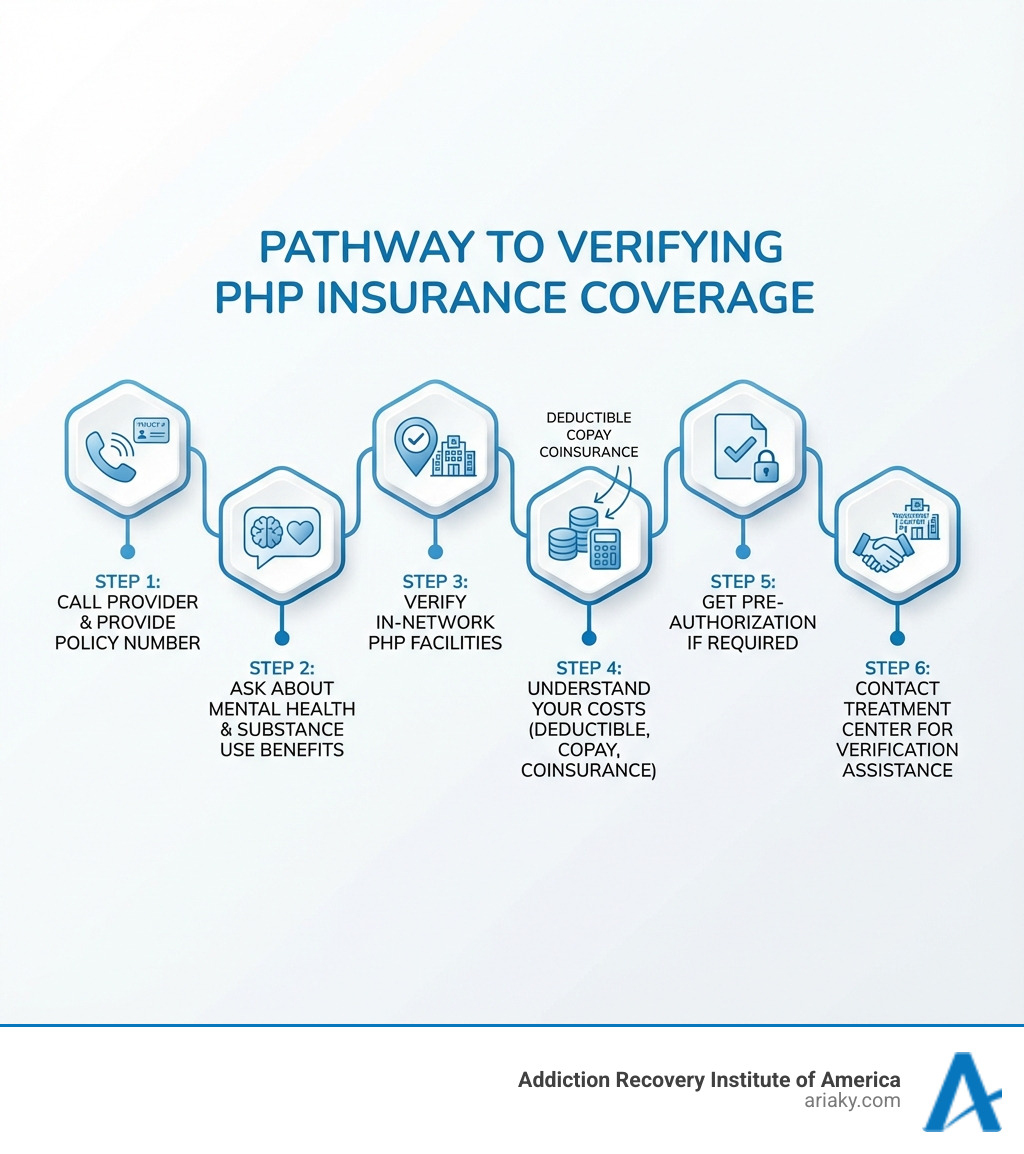
How to Verify if Your Insurance Covers a Partial Hospitalization Program
While federal laws mandate coverage, you must verify your specific benefits. This can be complex, but we can guide you.
The most direct way is to contact your insurance provider. You’ll find a customer service number on the back of your insurance card. When you call, be prepared with this helpful list of questions:
- What is my policy number and group number? (Have this ready when you call)
- What are my mental health and substance use disorder benefits?
- Does my plan cover Partial Hospitalization Programs (PHPs) for mental health and/or substance use treatment?
- What is my deductible, and has it been met for the current policy year? (The deductible is the amount you pay out-of-pocket before your insurance starts to cover costs).
- What is my copayment or coinsurance for PHP services? (A copayment is a fixed amount you pay; coinsurance is a percentage of the cost).
- What is my out-of-pocket maximum, and how much have I contributed towards it? (This is the most you’ll have to pay in a policy year).
- Are there any limitations on the number of days or sessions covered for PHP?
- Do I need a referral from a primary care physician?
- Is pre-authorization or prior authorization required for PHP services? If so, what is the process?
- Are there specific in-network facilities or providers I must use in Kentucky (or other locations like Ashland, Bowling Green, Covington, Florence, Lexington, Louisville, Morehead, Newport, Owensboro, Paducah, West Palm Beach)? (Using in-network providers typically results in lower out-of-pocket costs).
- What services within a PHP are covered (e.g., individual therapy, group therapy, medication management, medical supervision)?
- Are there any services typically excluded from PHP coverage (e.g., meals, transportation, certain holistic therapies)?
We also highly recommend contacting the treatment center. Facilities like Addiction Recovery Institute of America offer complimentary insurance verification services. Our admissions team can help you understand your benefits, manage pre-authorization, and clarify potential costs, saving you time and stress.
Understanding Your Specific Insurance Plan’s PHP Coverage
While federal laws lay a strong foundation for mental health and substance use disorder coverage, the specifics of how does your insurance cover a partial hospitalization program will ultimately depend on the type of plan you have. Whether it’s a private plan or a government-funded program, each has its own nuances. Major private insurance carriers like Blue Cross Blue Shield, Aetna Insurance, and Cigna all offer coverage, but the details can vary widely.
Private Insurance Plans (PPO, HMO, etc.)
Most individuals with private health insurance will have plans categorized as either a Preferred Provider Organization (PPO) or a Health Maintenance Organization (HMO), among others.
- In-Network vs. Out-of-Network Providers: This is often the biggest factor impacting your out-of-pocket costs.
- In-network facilities have a contract with your insurance company, meaning they’ve agreed to provide services at a negotiated rate. Using an in-network PHP will almost always result in lower costs for you.
- Out-of-network facilities do not have such a contract. Your plan may still cover a portion of the cost, but you’ll likely pay a higher percentage, and your deductible and out-of-pocket maximums might be different. Some plans, like certain PPOs, offer more flexibility for out-of-network care, while HMOs typically require you to stay within their network.
- Pre-authorization Process: For PHPs, private insurance plans almost always require pre-authorization or prior authorization. This means the treatment center, in collaboration with your referring physician, must submit documentation to your insurer demonstrating medical necessity before treatment begins. Without this, your claim could be denied.
- Utilization Review: Even after initial approval, insurance companies often conduct utilization reviews throughout your treatment. This is to ensure that the PHP remains medically necessary and that you are progressing as expected. This process can sometimes lead to requests for additional documentation or, in some cases, a determination that a lower level of care is more appropriate.
It’s crucial to understand the specifics of your plan, including any managed care organizations like Magellan Health Insurance that might administer your behavioral health benefits.
Medicare Coverage for PHP
Medicare, the federal health insurance program for people aged 65 or older and certain younger people with disabilities, also covers Partial Hospitalization Programs.
Medicare Part B covers mental health services, including PHP, when provided by a hospital outpatient department or a Medicare-certified Community Mental Health Center (CMHC). For Medicare to cover your PHP, both your doctor (or other qualified mental health professional) and the partial hospitalization program must “accept assignment.” This means they agree to accept the Medicare-approved amount as full payment for services.
Covered Services within a Medicare PHP typically include:
- Individual and group psychotherapy
- Occupational therapy as part of mental health treatment
- Services of other trained mental health staff
- Patient training and education about their condition
- Family counseling (primarily for the patient’s condition)
- Medically necessary diagnostic services
- Certain drugs and biologicals that cannot be self-administered
Services typically NOT covered by Medicare for PHPs include:
- Meals
- Transportation to or from services
- Social support groups (distinct from group psychotherapy)
- Testing or training for job skills not directly part of mental health treatment
For more detailed information, you can refer to the official Medicare guidance on mental health care (partial hospitalization) or download their publication, Medicare and Your Mental Health Benefits (PDF | 216 KB).
Medicaid and CHIP Coverage for PHP
Medicaid and the Children’s Health Insurance Program (CHIP) are joint federal and state programs that provide health coverage to low-income individuals and families.
Medicaid and CHIP do cover mental health, drug, and alcohol use treatment, including PHPs, but the specifics of coverage can vary significantly by state. This is because each state administers its own Medicaid program within federal guidelines. For instance, Kentucky Partial Hospitalization services covered by Medicaid will adhere to the state’s specific regulations regarding eligibility, covered services, and duration of treatment.
If you have Medicaid or CHIP, contact your state’s Medicaid office or your specific managed care organization (if you have one) to understand the exact benefits available for PHPs in your area, such as Kentucky. Our team at Addiction Recovery Institute of America can also assist you in understanding your Kentucky-specific Medicaid or CHIP benefits.
TRICARE and VA Health Care for PHP
For our military service members, veterans, and their families, TRICARE and VA Health Care provide critical support for mental health and substance use disorders.
TRICARE is the healthcare program for uniformed service members, retirees, and their families worldwide. TRICARE typically covers mental health, drug, or alcohol misuse programs, including PHPs. Coverage details, such as deductibles, copayments, and any referral requirements, will depend on your specific TRICARE plan (e.g., TRICARE Prime, TRICARE Select). We encourage you to learn more about TRICARE coverage by calling the number on the back of your card or looking online for your plan’s specific benefits.
VA Health Care provides comprehensive health services to eligible veterans. This includes extensive coverage for both drug and alcohol use treatment and mental health services. PHPs are generally covered by VA Health Care when deemed medically necessary. Veterans seeking PHP treatment should consult with their VA primary care provider or mental health specialist to understand the referral process and specific benefits available to them. Our team can also help veterans and their families steer these benefits.
What to Do When Insurance Isn’t Enough
Even with robust insurance coverage, you may encounter out-of-pocket costs like deductibles, copayments, or coinsurance. These costs can feel daunting, but don’t let them deter you from seeking the vital care you need. Your recovery is paramount, and solutions are often available to help manage these expenses.
What if your insurance doesn’t cover a partial hospitalization program?
In the rare case your plan doesn’t cover a PHP or if out-of-pocket costs are a barrier, don’t despair. Several alternative payment options exist:
- Sliding Scale Fees: Many treatment centers, including some at Addiction Recovery Institute of America, offer fees based on your income and ability to pay.
- Payment Plans: Facilities may work with you to set up an installment plan, allowing you to pay for treatment costs over time.
- Healthcare Loans: Specialized loans are available from various financial institutions specifically for healthcare expenses.
- Grants and Scholarships: Non-profit organizations and some treatment centers offer grants or scholarships to help cover treatment costs.
- Employee Assistance Programs (EAPs): Your workplace may offer an EAP that provides limited counseling or can refer you to covered services and provide some financial assistance.
- Crowdfunding and Donations: Platforms exist where you can raise funds from friends, family, and the wider community.
- Health Savings Accounts (HSAs) and Flexible Spending Accounts (FSAs): You can use pre-tax dollars from these accounts to pay for qualified medical expenses, including PHP treatment.
Communicate openly with the treatment center’s admissions team. At Addiction Recovery Institute of America, we are committed to helping you find a path to recovery and can discuss various paying for treatment options with you.
What PHP Services Are Typically Covered vs. Not Covered?
Understanding what your insurance plan will cover within a PHP is as important as knowing that PHPs are covered in general. Here’s a breakdown of common inclusions and exclusions:
Typically Covered Services within a PHP:
Most insurance plans, especially those compliant with federal parity laws, will cover the core therapeutic components of a PHP. This includes:
- Individual Therapy Program: One-on-one sessions with a licensed therapist to address specific issues and develop coping skills.
- Group Therapy Program KY: Therapist-facilitated sessions where participants share experiences and provide support.
- Medication-Assisted Treatment (MAT) and Medication Management: For opioid or alcohol use disorders, MAT may be covered, along with consultations for prescribing and monitoring psychiatric medications.
- Medical Supervision and Monitoring: Oversight by medical professionals to ensure safety and manage any co-occurring physical health issues.
- Psychoeducation: Educational sessions on addiction, mental health, triggers, and relapse prevention.
- Family Counseling: Sessions aimed at educating family members and improving communication to support recovery.
Services Typically NOT Covered (or only partially covered) by Insurance in a PHP:
While core therapeutic services are generally covered, some ancillary services might not be fully reimbursed:
- Meals: While many PHPs provide meals, these are often not covered by insurance. Medicare, for example, explicitly excludes meals.
- Transportation: Costs for getting to and from the facility are usually not covered.
- Certain Holistic Therapies: Coverage for therapies like yoga, art therapy, or acupuncture can be inconsistent. Some plans may offer partial coverage, but others may not cover them at all.
- Vocational Training or Job Skills Training: If not directly part of the mental health treatment plan, these are often excluded.
- Childcare: Costs for childcare while you attend the PHP are typically not covered.
It’s vital to clarify these details with your insurance provider and the treatment center’s financial team before beginning a PHP to avoid any surprises.
Take the Next Step Towards Healing in Kentucky
Navigating insurance and addiction treatment can feel like a labyrinth, but we hope this guide has shone a light on the path forward. The key takeaways are clear: does your insurance cover a partial hospitalization program? In most cases, yes, thanks to federal laws like the ACA and MHPAEA, which mandate coverage for mental health and substance use disorders as essential health benefits.
However, understanding the nuances of your specific plan—your deductible, copay, coinsurance, and whether a facility is in-network—is crucial. Medical necessity, certified by a qualified professional, is the gateway to approval, ensuring that you receive the appropriate level of intensive care.
At Addiction Recovery Institute of America, we believe that financial concerns should never be a barrier to receiving life-saving treatment. Whether you’re in Lexington, Louisville, Owensboro, Paducah, or any of our other Kentucky locations, our team is dedicated to helping you understand your options. We offer comprehensive Kentucky Drug Alcohol Rehab Programs and are here to assist you with verifying your benefits and exploring all available payment solutions.
If you or a loved one is struggling, peace is possible, and there are resources available to help you achieve it. Don’t let uncertainty hold you back from taking the next step. Reach out today to learn more about our Kentucky partial hospitalization services and let us help you start on your journey to lasting recovery. Your health, well-being, and future are worth it.

