Understanding Alcohol Withdrawal: A Critical Medical Condition
Alcohol wd (withdrawal) is a potentially life-threatening condition that occurs when someone with alcohol dependence suddenly stops or significantly reduces their drinking. This medical emergency affects approximately 50% of people with alcohol use disorder who quit drinking and can range from mild discomfort to severe, fatal complications.
Quick Facts About Alcohol Withdrawal:
- Timeline: Symptoms typically begin 6-24 hours after last drink
- Peak: Most intense symptoms occur 24-72 hours after stopping
- Duration: Acute phase lasts 5-7 days, some symptoms may persist weeks
- Severity: Ranges from mild (anxiety, tremors) to severe (seizures, delirium tremens)
- Risk: Delirium tremens affects 3-5% of cases with 5-25% mortality rate if untreated
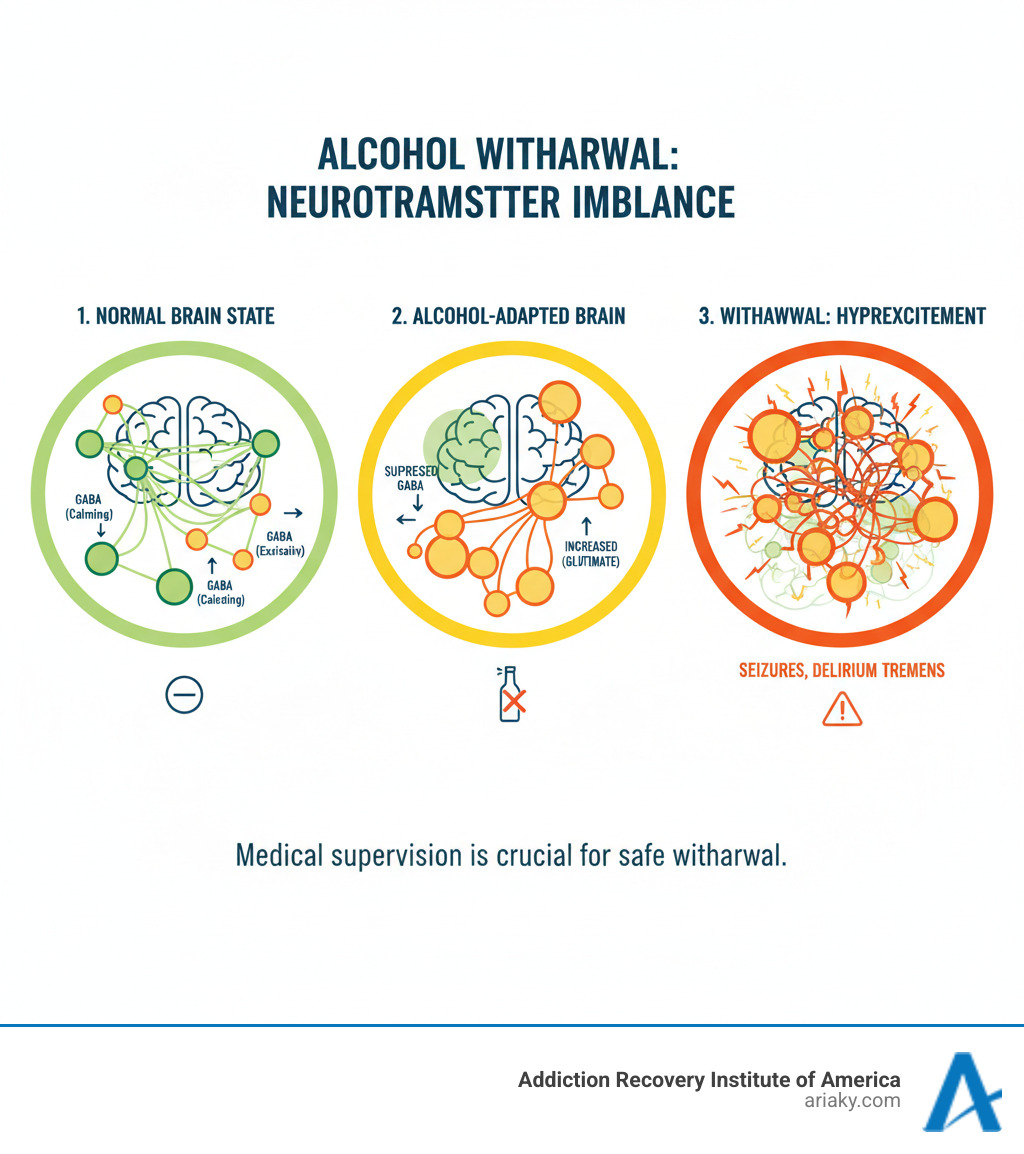
Alcohol withdrawal happens because chronic drinking alters brain chemistry. Alcohol suppresses your central nervous system, so your brain compensates by working harder to maintain normal function. When alcohol is removed, the brain remains in this hyperactive state. This creates dangerous symptoms as neurotransmitters like GABA and glutamate become severely imbalanced.
Crucially, alcohol withdrawal can be deadly. Unlike withdrawal from most other substances, stopping alcohol without medical supervision can cause fatal seizures and delirium tremens. This is why professional medical detox is essential for safety.
If you or a loved one are experiencing alcohol withdrawal symptoms, don’t try to manage it alone. With proper medical care, the success rate for safe withdrawal is extremely high, and it’s the crucial first step toward lasting recovery.
What Causes Alcohol Withdrawal and Who is at Risk?
When someone drinks heavily for weeks or months, their body becomes physically dependent. Alcohol wd happens because the brain has rewired itself to expect alcohol’s presence. This is a biological response, not a matter of willpower or weakness.
Understanding what happens after quitting alcohol can help you prepare for this challenging but temporary phase of recovery.
Why Does the Body React This Way?
As a central nervous system depressant, alcohol slows brain function by boosting GABA (a calming neurotransmitter) and suppressing glutamate (an excitatory one). Over time, the brain fights back by reducing its own GABA production and cranking up glutamate activity. This adaptation is why people develop tolerance and physiological dependence—the body now needs alcohol just to feel normal.
When you stop drinking, the brain is stuck in overdrive. The natural brakes (GABA) are weak, and the accelerator (glutamate) is floored. This neurotransmitter rebound creates a hyper-excitable state, causing symptoms that are the opposite of alcohol’s effects: anxiety, tremors, and potentially dangerous complications.
Key Risk Factors for Severe Withdrawal
Not everyone who stops drinking will face severe alcohol wd, but certain factors increase the risk of life-threatening complications.

- Drinking History: Heavy, daily alcohol use (typically 5+ drinks per day for men, 4+ for women) creates deeper physical dependence.
- Previous Withdrawals: A history of delirium tremens or seizures is a major red flag. Due to the kindling effect, each withdrawal episode can be more severe than the last.
- Age and Health: People over 65 and those with existing health problems like heart disease or abnormal liver function are at higher risk.
- Nutritional Deficiencies: Dehydration and electrolyte imbalances are common. Low levels of magnesium, potassium, and thiamine can trigger seizures.
- Co-occurring Conditions: Liver disease, heart problems, or other substance use issues add stress the body may not handle safely.
The more risk factors you have, the more critical it is to seek professional medical help for a safe withdrawal.
Understanding the Symptoms and Timeline of Alcohol WD
When someone with alcohol dependence stops drinking, their body goes through a predictable pattern of symptoms. Understanding this timeline helps you know what to expect and why medical supervision is vital. The symptoms of alcohol wd follow a fairly consistent progression, though each person’s experience is unique.
Healthcare professionals use tools like the CIWA-Ar scale (Clinical Institute Withdrawal Assessment for Alcohol, Revised) to measure symptom severity and determine the right level of care. The intensity and duration of withdrawal depend on how much and how long you’ve been drinking, your health, and previous withdrawal experiences. For a complete picture, our detailed Alcohol Withdrawal Timeline breaks down each phase.
Stage 1: Mild Symptoms (6-12 Hours)
The first signs of alcohol wd usually appear within 6 to 12 hours of the last drink. These early symptoms are uncomfortable but generally not dangerous. They include:
- Anxiety and nervousness: Feeling irritable, on edge, or having racing thoughts.
- Insomnia: Difficulty falling or staying asleep.
- Nausea and stomach upset.
- Headache.
- Heart palpitations: A pounding or racing heart.
- Tremors: Shakiness, especially in the hands (“the shakes”).
- Sweating.
For those with less severe dependence, symptoms may ease after 24 hours. For others, this is just the beginning.
Stage 2: Moderate Symptoms (12-48 Hours)
Symptoms typically intensify between 12 and 48 hours as the brain’s overactivity increases.
- Increased blood pressure and heart rate.
- Confusion and difficulty concentrating.
- Mild fever.
- Alcoholic hallucinosis: Seeing, hearing, or feeling things that are not there, while often retaining awareness that they are not real.
This 24 to 72-hour window is often when symptoms peak, making medical support critical for safety.
Stage 3: Severe Symptoms & Delirium Tremens (48-72+ Hours)
The most dangerous phase of alcohol wd can begin 48 to 72 hours after the last drink, sometimes later. This stage includes the risk of Delirium Tremens (DTs), a medical emergency.
Delirium Tremens (DTs) is the most serious form of withdrawal, affecting a small percentage of individuals but carrying a high mortality rate if untreated. With modern medical care, the fatality rate is low, but immediate treatment is required. Symptoms include:
- Profound confusion and disorientation.
- Extreme agitation and distress.
- High fever and drenching sweats.
- Vivid hallucinations that feel real, causing terror and panic.
- Grand mal seizures, which are most common 6 to 48 hours after the last drink.
- Unstable vital signs, including dangerous swings in heart rate and blood pressure that can lead to heart attack or stroke.
DTs symptoms usually peak around day four or five. The unpredictability of these severe complications is why attempting to detox alone is so risky. With proper medical supervision, even severe alcohol wd can be managed safely.
How Alcohol Withdrawal is Diagnosed and Treated
Diagnosing and treating alcohol wd requires a comprehensive approach to ensure your safety. The process begins with a thorough assessment by our medical team.
This includes a review of your drinking patterns, medical history, and current symptoms. We use the CIWA-Ar protocol, a standardized tool, to measure the severity of withdrawal symptoms like anxiety and tremors, which guides our treatment decisions. Blood tests are also crucial to check electrolyte levels, as imbalances in minerals like magnesium can increase seizure risk. We also run liver function tests and check for nutritional deficiencies, especially thiamine (vitamin B1), to prevent serious brain complications.
Based on this assessment, we determine the right level of care. While mild cases may be managed outpatient, most people with moderate to severe alcohol wd require inpatient medical supervision, like that provided in our Kentucky Detox program.
Medical Detoxification: The Safest Approach for Alcohol WD
Medical detox is often life-saving for alcohol wd due to its unpredictable and dangerous nature. 24/7 monitoring allows for immediate intervention if complications arise.
| Feature | Outpatient Medical Detox | Inpatient Medical Detox |
|---|---|---|
| Setting | Home, with daily visits to a clinic | Dedicated medical facility (e.g., hospital, rehab center) |
| Monitoring | Intermittent, daily check-ins | Continuous 24/7 medical supervision and observation |
| Severity Suited | Mild symptoms, no history of seizures/DTs, strong support system | Moderate to severe symptoms, history of seizures/DTs, co-occurring conditions |
| Medication | Prescribed for home use, with careful monitoring | Administered and adjusted by medical staff as needed |
| Safety | Lower safety for high-risk individuals | Highest safety, immediate response to complications |
| Support | Relies heavily on home support | Integrated medical, emotional, and therapeutic support |
The goal is to keep you safe and comfortable while your brain rebalances. We use specific medications to calm the overactive nervous system:
- Benzodiazepines (e.g., lorazepam, diazepam) are the first-line treatment. They improve the brain’s calming neurotransmitter (GABA) to reduce anxiety, stop tremors, and prevent seizures.
- Barbiturates like phenobarbital may be used for severe withdrawal, especially if benzodiazepines are not sufficient.
- Anticonvulsants like gabapentin help prevent seizures while also improving mood, sleep, and reducing cravings.
- Other supportive medications like beta-blockers can manage high blood pressure and rapid heart rate.
Our Alcohol Detox Program KY combines these medical interventions with compassionate care for a safe and supportive detox experience.
The Role of Supportive Care and Long-Term Treatment

Medication is only one part of managing alcohol wd. Comprehensive supportive care is vital.
- IV fluids and electrolyte correction rehydrate the body and restore essential minerals, which is crucial for preventing seizures.
- Thiamine supplementation is critical to prevent Wernicke-Korsakoff syndrome, a serious, alcohol-related brain disorder.
- Nutritional support helps your body heal and regain strength.
- A safe and supportive environment minimizes stress and promotes healing.
Detox is just the first step. Lasting recovery requires addressing the root causes of addiction.
- Counseling and behavioral therapies like CBT and DBT help you develop healthy coping skills.
- Support groups like Alcoholics Anonymous and SMART Recovery provide invaluable peer connection and a framework for sobriety.
- Medications for alcohol use disorder (e.g., naltrexone, acamprosate) can be prescribed after detox to help maintain sobriety.
Our Alcoholism Treatment Programs provide this full continuum of care, building a foundation for long-term success.
Frequently Asked Questions about Alcohol Withdrawal
It’s natural to have questions when facing alcohol wd. Here are clear, honest answers to some common concerns.
How long do alcohol withdrawal symptoms last?
The timeline for alcohol wd varies but generally follows a predictable pattern.
- The acute phase, with the most intense physical symptoms, typically lasts 5 to 7 days.
- Peak symptoms usually occur 24 to 72 hours after the last drink. This is the most critical window for medical supervision.
- Post-Acute Withdrawal Syndrome (PAWS) can cause lingering psychological symptoms like mood swings, anxiety, and sleep issues for weeks or even months. These symptoms fade over time with proper support.
Because individual variation is significant, your experience may be shorter or longer than someone else’s.
Can you die from alcohol withdrawal?
Yes, alcohol withdrawal can be fatal. Understanding this risk is critical for safety. The primary dangers are:
- Delirium Tremens (DTs): This is the most severe complication, causing extreme confusion, high fever, and unstable vital signs that can lead to heart attack or stroke. While modern treatment has lowered the mortality rate to around 1%, it is deadly without prompt medical care.
- Seizures: Grand mal seizures are a serious risk, especially in the first 48 hours, and can lead to injury or other complications.
- Cardiovascular Collapse: The extreme stress on the heart and blood vessels can become too much for the body to handle.
Call 911 immediately if you or someone else experiences seizures, high fever, severe confusion, hallucinations, or chest pain during withdrawal. These are medical emergencies. Detoxing from alcohol alone is extremely risky, which is why medical supervision is essential.
What is the ‘kindling effect’ in alcohol wd?
The kindling effect describes how repeated episodes of alcohol wd become progressively more severe. Each time you go through withdrawal, your brain becomes more sensitized to the absence of alcohol.
This means that every subsequent withdrawal tends to be more severe than the last, even if you haven’t been drinking more. The risk of dangerous complications like seizures and hallucinations increases, and symptoms may appear more quickly. This happens because of lasting changes in your brain’s chemistry.
The kindling effect underscores why preventing relapse is so crucial. Getting comprehensive treatment to achieve lasting sobriety helps protect you from increasingly dangerous future withdrawal episodes.
Your Path to Recovery Starts Here
The journey through alcohol wd should not be traveled alone. The risks of seizures and Delirium Tremens make professional medical support essential for your safety.
The good news is that recovery is absolutely possible. With proper medical care and comprehensive treatment, people successfully steer withdrawal and build fulfilling, alcohol-free lives. Those who engage in professional treatment have significantly better outcomes.
Preventing withdrawal complications starts with seeking help. Due to the kindling effect, each withdrawal can become more dangerous. Getting help now is the best decision for your long-term health. The prognosis with treatment is encouraging; medical supervision makes the acute phase safer, and ongoing support helps manage lingering symptoms.
At Addiction Recovery Institute of America (ARIA Kentucky), we believe every person deserves individualized care. As an accredited, AODE-certified addiction rehab center in Kentucky, our team will tailor a recovery journey specifically for you. Our continuum of care supports you from detox through to lasting recovery, offering medically supervised detox, residential treatment, PHP, and IOP to find the right level of care for your needs.
The Benefits of an Alcohol Rehab Center extend beyond safe withdrawal to include learning coping skills and building a lasting support network.
Your health and future are worth fighting for. Don’t let the fear of withdrawal keep you trapped in a cycle that puts your life at risk.
Ready to take that crucial first step? Take the first step toward a safe recovery at our alcohol detox program in Kentucky. Our team is here to answer your questions, address your concerns, and help you start this journey with the medical support and compassionate care you deserve.


