Why Understanding Your Detox Options Matters
Benzo detox centers are specialized medical facilities designed to safely manage benzodiazepine withdrawal under 24/7 supervision, but they’re not the right choice for everyone. If you took your prescription as directed and are physically dependent (not addicted), a slow, outpatient taper with your doctor may be safer and more appropriate than a traditional detox center.
When to Consider a Benzo Detox Center:
- You’re misusing benzos or mixing them with other substances
- You meet criteria for addiction (cravings, loss of control, continued use despite harm)
- You’ve tried to quit on your own and relapsed
- You need immediate medical supervision due to severe dependence
- You have co-occurring mental health or substance use disorders
When a Slow Taper May Be Better:
- You’ve taken benzos as prescribed by your doctor
- You’re physically dependent but not addicted
- You can commit to a gradual reduction over months or years
- You have access to a knowledgeable prescriber
- You don’t have a history of polysubstance abuse
Benzodiazepines are central nervous system depressants commonly prescribed for anxiety, insomnia, and seizures. Common brands include Xanax (alprazolam), Valium (diazepam), and Klonopin (clonazepam). According to the 2021 National Survey on Drug Use and Health, more than 25 million people aged 12 and older used prescription benzodiazepines, while 3.9 million people misused them.
The core dilemma many people face is this: Should I go to a detox center, or should I work with my doctor on a slow taper? The answer depends entirely on whether you’re dealing with physical dependence from prescribed use or true addiction involving compulsive behaviors.
This distinction matters because traditional detox and rehab facilities often use a 12-step addiction model that focuses on abstinence and behavioral change. While this approach works well for substance use disorders, it can be inappropriate—and even dangerous—for compliant patients who simply need medical guidance to safely discontinue a prescribed medication.
Withdrawal from benzodiazepines can be severe and potentially life-threatening. Symptoms can include anxiety, insomnia, tremors, seizures, and in rare cases, psychosis or death. This is why medical supervision is critical, regardless of which path you choose.
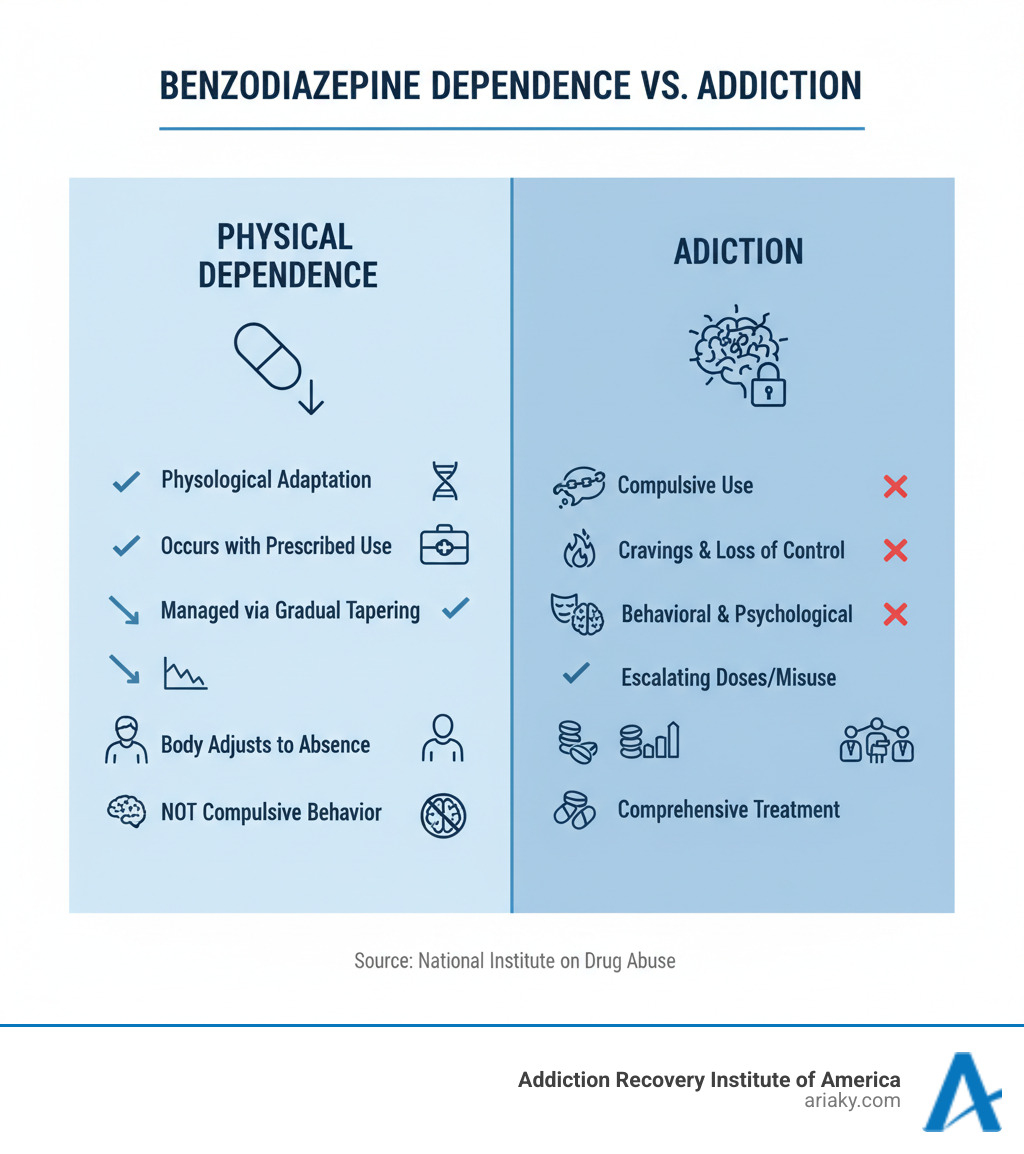
Understanding Benzodiazepine Dependence vs. Addiction
If you’re thinking about stopping benzodiazepines, there’s one crucial distinction you need to understand first: the difference between physical dependence and addiction. These terms get tossed around interchangeably, but they describe very different experiences—and each requires its own approach to treatment.
Physical dependence is simply your body’s natural adaptation to a medication. It’s not a character flaw or a sign of weakness. When you take benzodiazepines regularly over time, your brain chemistry adjusts to their presence. If you suddenly stop or cut back too quickly, your body responds with withdrawal symptoms. This happens even if you’ve taken your medication exactly as prescribed, never taken an extra pill, and never felt “high” from it. As the National Institute on Drug Abuse explains, physical dependence and addiction are not synonymous.
Many people develop what doctors call iatrogenic dependence—physical dependence caused by medical treatment itself. Maybe you started taking Xanax for panic attacks five years ago, following your doctor’s instructions perfectly. Your body adapted to the medication, and now you can’t just stop without consequences. This doesn’t make you an addict. It makes you someone who needs medical guidance to safely taper off a medication your body has grown accustomed to. Benzo detox centers that specialize in addiction recovery may not be the right fit for this situation.
Addiction—or what clinicians call Substance Use Disorder—is something fundamentally different. It’s a complex condition characterized by compulsive drug seeking and use despite serious negative consequences. The DSM-5 outlines specific criteria that go far beyond physical dependence. We’re talking about patterns like obsessing over the drug, repeatedly failing to quit, experiencing intense cravings, neglecting important responsibilities, and continuing to use even when it’s clearly damaging your health, relationships, or career.
Tolerance adds another layer of complexity here. When you develop tolerance, you need higher doses to get the same effect. This can happen with both physical dependence and addiction, but the context matters enormously. If you’re taking prescribed benzos and notice they’re not working as well, that’s tolerance. If you’re crushing and snorting extra pills to chase a high, that’s addiction. Unfortunately, some prescribers don’t understand this distinction and automatically assume that evidence of tolerance and withdrawal symptoms means a patient is addicted, which can lead to inappropriate treatment recommendations.
Here’s a comparison that might help clarify:
| Feature | Physical Dependence (Prescribed Use) | Addiction (Misuse) |
|---|---|---|
| How it develops | Predictable physiological adaptation to regular use | Compulsive use despite negative consequences |
| Medication source | Prescribed by doctor, taken as directed | Often involves doctor shopping, buying pills illegally, or taking someone else’s prescription |
| Behavior patterns | No drug-seeking behavior or cravings | Obsessive thoughts about the drug, loss of control over use |
| Dose escalation | May need adjustments over time for medical reasons | Frequently takes more than prescribed to get high or cope |
| Treatment approach | Gradual medical taper under doctor supervision | Comprehensive addiction treatment including behavioral therapy and possibly benzo detox centers |
| Underlying issue | Body needs time to readjust to absence of drug | Requires addressing psychological, behavioral, and social factors driving compulsive use |
Signs and Symptoms of Benzodiazepine Addiction
So how do you know if you’ve crossed the line from dependence to addiction? The behavioral signs are usually pretty clear once you know what to look for.
Doctor shopping is a major red flag—visiting multiple doctors to get multiple prescriptions for the same medication. If you’re taking more than prescribed regularly, even if you tell yourself it’s just because you “really need it,” that’s a warning sign. Intense cravings that dominate your thoughts, neglecting work or family responsibilities because of your benzo use, and continuing to take the medication even though it’s causing obvious problems in your life all point toward addiction rather than simple dependence.
Mixing benzodiazepines with other substances is particularly dangerous and often indicates a substance use disorder. Combining benzos with alcohol or opioids dramatically increases the risk of overdose and death. If you’re using benzos alongside other drugs—whether that’s heroin, prescription opioids, or alcohol—you need specialized addiction treatment, not just a simple medication taper.
The distinction between dependence and addiction isn’t just academic. It determines whether you need a slow outpatient taper with your regular doctor or comprehensive treatment at a facility equipped to address the complex behavioral and psychological aspects of addiction. Getting this right from the start can make the difference between a successful recovery and a dangerous detox experience.
Understanding Benzodiazepine Dependence vs. Addiction
If you’ve been taking benzodiazepines for a while, you might feel trapped between two fears: “Am I addicted?” and “What happens if I stop?” The truth is, what you’re experiencing might not be addiction at all—and understanding the difference could completely change how you approach getting off these medications.
Physical dependence is simply your body’s natural response to having a medication in your system regularly. Think of it like this: if you drink coffee every morning for months, then suddenly stop, you’ll probably get a headache. That doesn’t make you a coffee addict—it just means your body got used to the caffeine. The same principle applies to benzodiazepines, except the stakes are much higher. When you take benzos consistently, your brain chemistry adjusts to their presence. Stop abruptly, and your body reacts with withdrawal symptoms. This can happen even if you never took more than your doctor prescribed.
Many people develop what’s called iatrogenic dependence—a medical term that means “caused by medical treatment.” You followed your doctor’s orders. You took your Xanax or Klonopin exactly as prescribed for anxiety or insomnia. And now your body depends on it. This isn’t a character flaw or a sign that you’ve done something wrong. As the National Institute on Drug Abuse makes clear, physical dependence and addiction are not synonymous.
Addiction—or what clinicians call Substance Use Disorder—is something entirely different. It’s a complex condition where you continue using a substance compulsively, even when it’s causing serious problems in your life. The DSM-5 (the manual mental health professionals use for diagnosis) outlines specific criteria that go far beyond just experiencing withdrawal symptoms.
With addiction, you’ll see behavioral signs that cross a line: obsessing about the drug, using it in ways that weren’t intended, continuing despite obvious harm, and losing control over your use. You might find yourself taking more than prescribed, seeking pills from multiple doctors, or mixing benzos with alcohol or other drugs to chase a certain feeling. Your relationships suffer. Your work performance drops. You know it’s a problem, but you can’t seem to stop.
Tolerance is another piece of the puzzle, and it can be confusing because it happens in both scenarios. Tolerance simply means you need more of the drug to get the same effect. If you’re physically dependent from prescribed use, you might notice your anxiety isn’t as well-controlled as it used to be. If you’re dealing with addiction, tolerance often drives you to take increasingly dangerous amounts or combine substances.
Here’s a side-by-side look at how these two conditions differ:
| Feature | Physical Dependence (Prescribed Use) | Addiction (Misuse) |
|---|---|---|
| Cause | Natural adaptation to prescribed medication | Compulsive drug-seeking behavior despite harm |
| Behavior | Taking medication as directed | Taking more than prescribed, doctor shopping, mixing substances |
| Control | Can follow medical guidance | Loss of control over use |
| Consequences | Withdrawal if stopped suddenly | Continued use despite negative impacts on health, relationships, work |
| Treatment approach | Gradual taper with doctor supervision | Comprehensive behavioral treatment plus medical detox |
| Focus | Managing physiological withdrawal | Addressing underlying psychological and behavioral patterns |
This distinction matters tremendously when you’re considering benzo detox centers versus working with your prescribing doctor. If you’re physically dependent but not addicted, a traditional detox facility focused on the 12-step addiction model might not be the right fit. You need medical guidance to safely reduce your dose over time, not intensive behavioral therapy for compulsive use.
On the other hand, if you’re experiencing true addiction—if you’ve been misusing benzos, combining them with alcohol or opioids, or exhibiting compulsive behaviors around the drug—then a comprehensive treatment program at a benzo detox center could be lifesaving.
Signs and Symptoms of Benzodiazepine Addiction
So how do you know if you’ve crossed from dependence into addiction territory? The behavioral signs are usually the clearest indicators.
Doctor shopping is a major red flag. If you’re visiting multiple physicians to get extra prescriptions, or if you’ve lied to a doctor about losing your pills, that’s not typical dependence behavior. Similarly, consistently using more than prescribed—taking extra pills on stressful days, or finishing your monthly prescription in two weeks—suggests a loss of control.
Cravings are another telling sign. Physical dependence might make you anxious about running out of medication, but addiction involves an intense, consuming desire for the drug itself. You think about it constantly. You plan your day around it.
When benzos start interfering with your life, that’s when alarm bells should ring. Are you neglecting responsibilities at work or home? Missing important events because you’re too sedated? Have relationships suffered because of your use? These are classic addiction patterns.
Perhaps most concerning is continued use despite negative consequences. You know the benzos are causing problems—maybe you’ve had blackouts, dangerous falls, or your doctor has warned you about liver damage—but you keep taking them anyway. That’s the hallmark of addiction.
Mixing benzos with other substances is extremely dangerous and often indicates a substance use disorder. Combining benzodiazepines with alcohol amplifies the sedative effects and can be fatal. Mixing them with opioids is even more deadly—both are central nervous system depressants, and together they can stop your breathing. If you’ve been combining benzos with heroin or prescription painkillers, you need professional help immediately.
The good news is that whether you’re dealing with physical dependence or full-blown addiction, there’s a safe path forward. Understanding which one you’re facing is the first step toward getting the right kind of help—whether that’s a carefully managed taper with your doctor or comprehensive treatment at a facility that specializes in benzodiazepine recovery.

