Why Bowling Green Drug Rehab is Essential for Our Community
Bowling green drug rehab services have become a critical lifeline in Kentucky’s fight against the growing substance use crisis. If you’re searching for addiction treatment in the Bowling Green area, here are your main options:
Types of Treatment Available:
- Medical Detox – Safe, supervised withdrawal from substances
- Inpatient/Residential – 24/7 care in a treatment facility
- Partial Hospitalization (PHP) – Day treatment with evening home stays
- Intensive Outpatient (IOP) – Several therapy sessions per week
- Standard Outpatient – Weekly counseling sessions
Payment Options:
- Private insurance (often covers 50-100% of costs)
- Kentucky Medicaid and Medicare
- Sliding scale fees
- Private pay arrangements
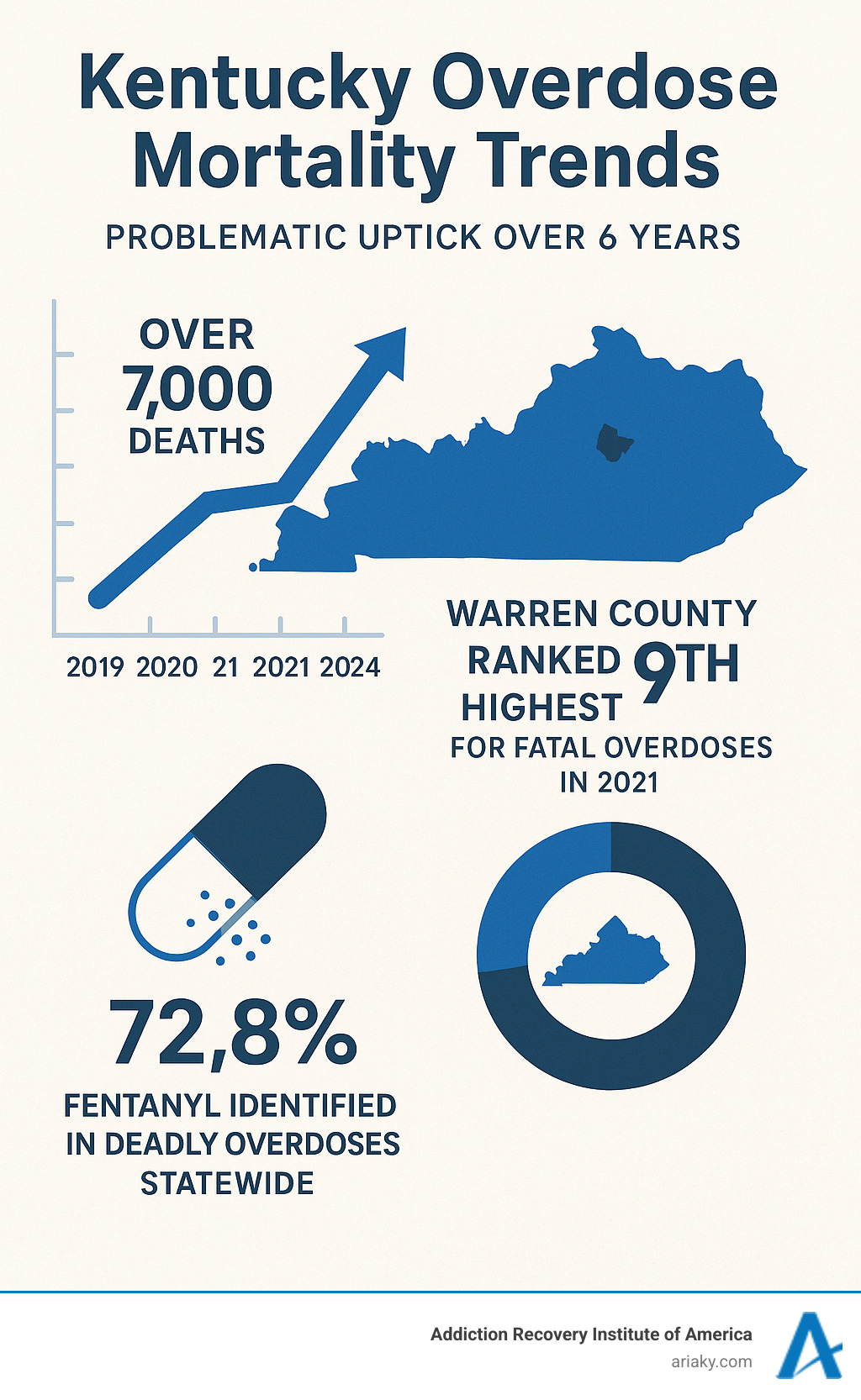
The statistics paint a sobering picture of addiction’s impact on our community. Between 2019 and 2020, overdose deaths in our area increased from 21 to 25, then jumped to 36 in 2021. Warren County now ranks ninth in Kentucky for fatal overdoses, with fentanyl identified in over 72% of deadly overdoses statewide.
But there’s hope. Kentucky ranks among the top states for available addiction treatment centers per capita. Local facilities offer everything from same-day admissions to long-term recovery support.
“I was terrified to go to rehab but found the experience warm and welcoming, with staff ensuring my needs were met,” shared one Bowling Green treatment center alumni.
Recovery is possible when you have the right support and treatment approach.
The Reality of Addiction in Bowling Green and Kentucky
Bowling Green has earned recognition from Money Magazine and Times magazine as a wonderful place to live. Yet beneath this positive reputation lies a sobering truth that touches families throughout our community. Substance use disorder doesn’t discriminate – it affects people from all walks of life, and the numbers tell a story we can’t ignore.
Since 2014, Kentucky has seen the opioid overdose death rate climb to 20 per 100,000 people. These aren’t just statistics on a page – they represent our neighbors, coworkers, and loved ones. The gender disparity is particularly striking: while women face just over 10 opioid deaths per 100,000, men experience nearly 25 deaths per 100,000.
The scope of Kentucky’s crisis becomes even clearer when you look at the bigger picture. Over the past six years, more than 7,000 Kentuckians have lost their lives to overdose. In 2019 alone, over 1,300 families said goodbye to someone they loved. By September 2020, nearly 2,000 people had died from substance overdoses across our state.
Our state ranked 7th nationally for overdose rates in 2019, with 32.5 deaths per 100,000 people. Right here in Warren County, we faced the ninth-highest number of fatal overdoses in Kentucky during 2021. The presence of fentanyl has made this crisis even more dangerous – it was identified in nearly 73% of all deadly overdoses statewide last year.
Between 2015 and 2019, Warren County tragically lost 82 people to overdoses. These losses ripple through our entire community, affecting families, friends, and everyone who knew these individuals.
The impact extends far beyond overdoses. Warren County recorded 1,955 drug and narcotics offenses in 2019, putting strain on our law enforcement and court systems. Alcohol abuse adds another layer of community harm, with over 4,700 alcohol-related vehicle collisions across Kentucky in 2019. These crashes resulted in 2,432 injuries and claimed 140 lives.
These realities underscore why bowling green drug rehab services aren’t just helpful – they’re absolutely essential for protecting and healing our community. Understanding the scope of this challenge helps us recognize why accessible, quality treatment matters so much.
For deeper insight into our state’s struggles, these resources provide valuable context:
Recognizing the Signs of Addiction
Addiction can be sneaky. It often starts small and grows gradually, making it hard to spot at first. Recognizing the warning signs early can make all the difference in getting help for yourself or someone you care about.
The changes usually show up in different areas of a person’s life. Behavioral shifts are often the first things family members notice. Someone might become more secretive or start lying about where they’ve been. They may abandon old friends for a new crowd, or lose interest in hobbies and activities they once loved. Responsibilities start slipping – work performance drops, school attendance becomes spotty, or household duties get ignored.
Physical symptoms vary depending on what substances are involved, but common signs include dramatic weight changes, poor personal hygiene, and unusual pupils – either very large or very small. You might notice bloodshot eyes, tremors, or coordination problems. Strange smells on their breath or clothing can also be telltale signs.
Psychological changes can be just as telling. Mood swings become more frequent and intense. Someone who was once even-tempered might become irritable, anxious, or depressed without obvious reason. Social withdrawal often follows – they pull away from family gatherings, stop returning calls, and prefer isolation.
Neglecting responsibilities becomes a pattern. Bills go unpaid, important appointments get missed, and commitments are broken. Financial problems often emerge as money gets redirected toward obtaining substances instead of covering necessities.
If you’re seeing these signs in someone you care about, addiction is a disease, not a character flaw. Approaching the situation with compassion rather than judgment opens the door for honest conversation and, hopefully, treatment.
The Scope of the Problem in Our Community
Behind every statistic we’ve shared lives a human story. When we talk about Warren County’s 82 overdose deaths between 2015 and 2019, we’re talking about 82 empty chairs at dinner tables. These numbers from Warren County Fentanyl Death Statistics represent parents who will never see their children graduate, kids who grew up without a mom or dad, and spouses learning to steer life alone.
The 1,955 drug and narcotics offenses in Warren County during 2019 show how addiction creates ripple effects throughout our community. These aren’t just legal problems – they represent families in crisis, children who might end up in foster care, and neighborhoods dealing with increased crime and safety concerns.
Families bear the heaviest burden. We see parents desperately trying to help an adult child who keeps relapsing. Children struggle to understand why mommy or daddy acts so differently. Grandparents find themselves raising grandchildren because addiction has made their own children unable to parent effectively.
Kentucky has recognized these challenges and responded with innovative programs. Drug courts work to keep families together by focusing on treatment rather than just punishment. Special training helps teachers understand children who were born to parents with addiction. Caseworkers receive advanced education about the unique needs of foster children, who face higher risks of developing substance use problems themselves.
Child endangerment cases often trace back to parental addiction, creating cycles that can span generations. When parents can’t provide safe, stable homes due to their substance use, children suffer trauma that may increase their own addiction risk later in life.
This isn’t just Bowling Green’s problem – it’s part of a statewide crisis that affects communities across Kentucky. But here’s some encouraging news: Kentucky also leads the nation in providing solutions. Our state ranks among the highest for addiction treatment center availability per capita.
That means hope and help are available right here in our community. The same forces that created this crisis – our close-knit community connections and Kentucky’s commitment to caring for our own – are now working to provide pathways to recovery.
Understanding the Levels of Care in Addiction Treatment
Finding the right Bowling Green drug rehab program can feel overwhelming, especially when you’re already dealing with the challenges of addiction. The good news is that there’s a structured approach to help you find exactly what you need. Think of addiction treatment like a ladder – you start where you need to start, and you can move up or down based on how you’re doing.
At ARIA Kentucky, we use something called the ASAM criteria – that’s the American Society of Addiction Medicine’s guidelines. These aren’t just fancy rules; they’re like a roadmap that helps us figure out what level of care will work best for you. Maybe you need intensive, round-the-clock support, or perhaps you’re ready for something that lets you keep working while you heal. There’s no shame in needing more support, and there’s no rush to need less.
This approach is called a “continuum of care,” which simply means your treatment can change as you change. You might start in a residential program and gradually step down to outpatient care as you build confidence and coping skills. Or maybe you’ll find that you need to step back up to a more intensive level – and that’s perfectly okay too. Recovery isn’t a straight line, and neither is treatment.
What makes this work is that it’s completely individualized. Your story, your struggles, your strengths – they’re all different from the next person’s. That’s why cookie-cutter approaches don’t work for something as personal as addiction recovery.
For more information on the comprehensive programs available, visit Kentucky Drug and Alcohol Rehab Programs.
Medical Detoxification
Before we can really dive into the healing work of recovery, your body needs to be stable. That’s where medical detoxification comes in – and the word “medical” is really important here. This isn’t about toughing it out alone or trying to detox at home. Withdrawing from certain substances, especially alcohol and benzodiazepines, can actually be dangerous without proper medical supervision.
During medical detox, you’re not just getting through withdrawal – you’re being carefully monitored by medical professionals who know exactly what to watch for. Withdrawal symptoms can range from uncomfortable (like nausea and sweating) to potentially serious (like seizures or severe anxiety). Our medical team is there to manage these symptoms, often with medications that make the process much more comfortable and safe.
Here’s something important to understand: detox is just the beginning, not the whole journey. Think of it like clearing the fog so you can see the road ahead. Once your body is stable and your mind is clearer, that’s when the real work of recovery can begin. You’ll be ready to fully participate in therapy, learn new coping skills, and start building the foundation for lasting sobriety.
For people dealing with opioid addiction, we also offer Medication-Assisted Treatment (MAT). This might include medications like methadone or buprenorphine, which help manage cravings and withdrawal symptoms as part of a comprehensive treatment plan. It’s not trading one addiction for another – it’s using proven medical tools to help your brain heal.
To learn more about our medically supervised detox programs, please visit:
Inpatient and Outpatient Programs
Once detox is complete – or if detox isn’t medically necessary – you’ll move into the heart of addiction treatment. This is where that continuum of care really shows its value. At ARIA Kentucky, we offer several different levels of intensity, each designed to meet you exactly where you are in your recovery journey.
Residential treatment is our most comprehensive program. You’ll live at the facility and receive 24/7 medical care, therapy, and support. This level of care is ideal if you’re dealing with severe addiction, need a completely safe environment away from triggers, or have co-occurring mental health issues that require intensive attention. There’s something powerful about being surrounded by people who understand what you’re going through, all working toward the same goal.
Partial Hospitalization Programs (PHP) offer what many people call “intensive rehab.” You’ll spend several hours a day, multiple days a week in treatment, but you get to go home in the evenings. This works well if you need high-level care but can maintain your sobriety outside the facility, or if you’re stepping down from residential treatment and building confidence in managing recovery on your own.
Intensive Outpatient Programs (IOP) provide several therapy sessions per week while allowing you to maintain work, school, or family responsibilities. This level is perfect for people who have some stability but still need regular, structured support and accountability.
Standard Outpatient treatment typically involves weekly counseling sessions. This might be where you start if your addiction is less severe, or where you step down to as you build more independence in your recovery.
The beauty of this system is its flexibility. Life happens, stress occurs, and sometimes you need to adjust your level of care. That’s not failure – that’s smart recovery planning.
To learn more about each program level, visit:


