Why Safe Opioid Withdrawal Matters
Safe opioid withdrawal requires medical supervision, a gradual tapering plan, and ongoing support to prevent serious complications like uncontrolled pain, dangerous relapse, and overdose death. Many people who want to stop using opioids don’t realize how dangerous it is to quit suddenly.
Key components of safe withdrawal:
- Medical supervision: 24/7 monitoring by healthcare professionals.
- Gradual tapering: Reducing doses by 10-25% every 2-4 weeks.
- Medication support: Using buprenorphine, methadone, or clonidine to ease symptoms.
- Psychological care: Counseling and mental health support.
- Follow-up treatment: Continuing care after detox to prevent relapse.
After regular use, your body becomes physically dependent on opioids. Stopping abruptly triggers severe withdrawal symptoms, uncontrolled pain, psychological distress, and even suicidal thoughts. This is why the FDA now requires warning labels on opioids about the dangers of sudden discontinuation.
Physical dependence is not the same as addiction, but both require professional help to address safely.
The good news is that medically supervised withdrawal dramatically reduces these risks. Healthcare professionals create a patient-specific tapering plan based on your dose, duration of use, pain type, and overall health. This process is about biology and smart medical care, not willpower.
Understanding Opioid Withdrawal: Symptoms and Major Risks
When you take opioids regularly, your body adapts and develops physical dependence. This is a biological process, not a moral failing. If you suddenly stop, your body reacts strongly with opioid withdrawal syndrome, a condition that ranges from deeply uncomfortable to dangerous.
Opioids are depressants; during withdrawal, your body rebounds, sending everything into overdrive. To learn more about how they work, explore our resources on Opiates.
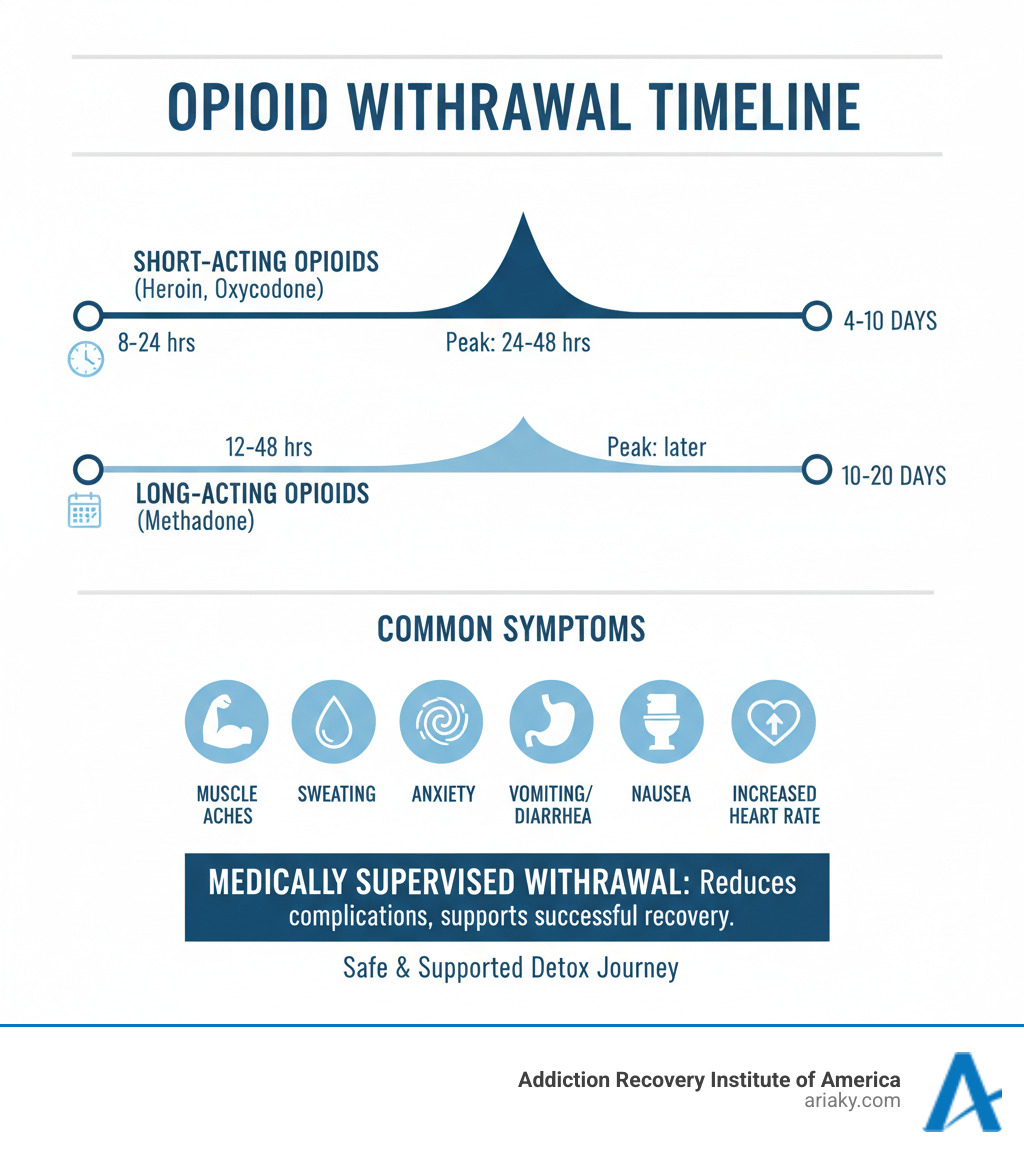
The withdrawal timeline depends on the opioid type:
- Short-acting opioids (heroin, oxycodone): Symptoms begin in 8-24 hours, peak within 24-48 hours, and last 4-10 days.
- Long-acting opioids (methadone): Symptoms begin in 12-48 hours and can last 10-20 days or more.
Even after physical symptoms fade, psychological distress like cravings and anxiety can linger for months. This is why safe opioid withdrawal is critical and why opioids are among the Most Addictive Substances.
The Dangers of Quitting “Cold Turkey”
Quitting opioids abruptly is dangerous. The FDA has documented serious harm from patients who stopped suddenly. Key risks include:
- Uncontrolled Pain: Especially for those with chronic pain, it can return more than before.
- Psychological Distress: Severe anxiety and dysphoria can lead to suicidal thoughts. This is a medical complication requiring immediate attention.
- Use of Illicit Opioids: To escape unbearable symptoms, some turn to street drugs like heroin, which are often laced with deadly fentanyl.
- Dehydration: Severe vomiting and diarrhea can cause life-threatening fluid and electrolyte loss. While less common than with alcohol withdrawal (see Delirium Tremens), it remains a serious risk.
- Overdose on Relapse: After abstinence, opioid tolerance drops significantly. Using the same previous dose can be fatal.
Key Signs and Symptoms to Monitor
Recognizing withdrawal symptoms helps you know when to seek help. Common signs include:
- Physical Discomfort: Deep muscle aches, cramps, and restlessness (the origin of “kicking the habit”).
- Digestive Issues: Nausea, vomiting, and severe diarrhea.
- Emotional Distress: Intense anxiety, irritability, and insomnia.
- Autonomic Symptoms: Alternating sweats and chills, goosebumps (piloerection), increased heart rate, and high blood pressure.
- Other Telltale Signs: Uncontrollable yawning, runny nose, tearing eyes, and dilated pupils.
While these symptoms are not typically life-threatening on their own, the associated risks—dehydration, psychological distress, and relapse—make unmonitored withdrawal extremely dangerous. Professional support, like that found in our Drug Detox Kentucky programs, is essential for safety.
The Foundation of Safe Opioid Withdrawal: Medically Supervised Tapering
Safe opioid withdrawal is best achieved through medically supervised tapering. This process involves slowly reducing your opioid dose over time, giving your body a chance to adjust at each step. It is the safe and effective alternative to abrupt discontinuation.

A healthcare team acts as your guide, creating a patient-specific tapering plan and monitoring your progress. They manage withdrawal symptoms, control pain, and provide education. Your role is to communicate openly, follow the plan, and report any concerning symptoms, such as increased pain or thoughts of self-harm. This partnership is the key to a safe withdrawal.
Programs like Drug Detox Kentucky provide this structured environment. For more details on tapering, the Mayo Clinic offers excellent resources on tapering off opioids.
Creating a Plan for a Safe Opioid Withdrawal
A safe tapering plan is built for you. The process begins with a thorough assessment of your medical and mental health history, support system, and the dose and duration of your opioid use. Your type of pain is also a critical factor, as alternative pain management strategies must be in place.
The tapering schedule is flexible but often follows a guideline of reducing the dose by 10-25% every 2-4 weeks. Slower tapers may be necessary for long-term users or at lower doses. The key is adjusting the plan based on your response.
Never suddenly stop taking your opioid medication without medical guidance. Work with your doctor to create a gradual plan. This is about biology and safety, not willpower. An Opioid Detox Program provides the necessary supervision.
The Difference Between Medically Supervised and Abrupt Discontinuation
The choice between a supervised taper and quitting “cold turkey” has vastly different outcomes.
| Feature | Medically Supervised Withdrawal | Abrupt Discontinuation (“Cold Turkey”) |
|---|---|---|
| Safety | High: Monitored by professionals, risks minimized. | Low: High risk of severe complications, life-threatening. |
| Symptom Management | Effective: Medications and supportive care alleviate symptoms. | Ineffective: Intense, unmanaged withdrawal symptoms. |
| Comfort Level | Increased: Symptoms are reduced, making the process tolerable. | Extremely Low: Unbearable physical and psychological distress. |
| Success Rate | Higher: Better chance of completing detox and engaging in treatment. | Very Low: High likelihood of relapse due to severe discomfort. |
| Overdose Risk | Reduced: Gradual tapering prevents loss of tolerance, naloxone available. | Increased: Loss of tolerance makes relapse highly dangerous. |
| Medical Emergencies | Prevented/Managed: Professionals intervene quickly if complications arise. | High Risk: Unforeseen complications can become medical emergencies. |
| Psychological Support | Integrated: Counseling and emotional support are part of the process. | Absent: No professional support for mental distress. |
| Transition to Treatment | Seamless: Detox is the first step to ongoing recovery programs. | Disconnected: Often leads back to opioid use, not treatment. |
Medically supervised withdrawal provides a safe, supportive, and effective path toward recovery, seamlessly connecting you to ongoing treatment. It is the clear choice for anyone serious about overcoming opioid dependence. To explore which treatment setting is right for you, learn about Inpatient vs Outpatient options.
Managing Symptoms with Medication-Assisted Treatment (MAT) and Support
Safe opioid withdrawal involves more than just enduring discomfort; it requires supporting the body and mind. Medication-Assisted Treatment (MAT) is a comprehensive approach that combines FDA-approved medications with counseling and behavioral therapies.
MAT is not swapping one drug for another. It uses medical tools to stabilize body chemistry, reduce cravings, and manage withdrawal symptoms while you build skills for lasting recovery. Research from sources like SAMHSA confirms that MAT is highly effective. Our Medication Assisted Treatment program at ARIA Kentucky integrates this approach with compassionate care.

The Role of Medication in a Safe Opioid Withdrawal
Medications are powerful tools for making withdrawal safer and more tolerable.
- Buprenorphine: A partial opioid agonist that relieves withdrawal and cravings without a strong high. It is often combined with naloxone (e.g., Suboxone) to prevent misuse.
- Methadone: A full opioid agonist used for decades to suppress withdrawal symptoms and cravings, typically administered in specialized programs.
- Lofexidine (Lucemyra): A non-opioid medication that reduces symptoms like muscle spasms, cramps, and anxiety by decreasing noradrenaline release.
- Clonidine: Another non-opioid that calms autonomic symptoms like sweating, chills, and muscle aches. It requires blood pressure monitoring.
- Adjunctive Medications: Other medications are used to target specific symptoms, such as anti-nausea drugs, pain relievers, and sleep aids.
The Mainstreaming Addiction Treatment (MAT) Act of 2023 removed the “X-Waiver,” making it easier for DEA-registered practitioners to prescribe buprenorphine and increasing access to care. Our Heroin Detox Program uses these evidence-based approaches for a safe detox.
Alternative Pain Management and Supportive Care
A holistic approach is essential for a truly safe opioid withdrawal. If you started opioids for chronic pain, alternative management is key. This includes physical therapy, acupuncture, massage, and chiropractic care. Mind-body techniques like yoga, meditation, and tai chi can also reduce pain and stress.
Mental health counseling is vital for addressing underlying conditions like depression or anxiety that often co-occur with opioid use disorder. Peer support groups like Narcotics Anonymous provide a community of people with shared experiences.
Finally, basic self-care is crucial. Staying hydrated and eating nutritious food supports your body’s healing process. Gentle lifestyle adjustments, such as moderate exercise and relaxation techniques, can also improve your well-being. At ARIA Kentucky, our Kentucky Addiction Treatment Therapy Programs treat the whole person—body, mind, and spirit.
Navigating Special Considerations and Long-Term Recovery
Completing the acute phase of safe opioid withdrawal is the starting line, not the finish. Recovery is an ongoing journey that requires continued effort, specialized care, and a solid aftercare plan to manage the high risk of relapse. Because your tolerance has dropped, a relapse can be especially dangerous.
For more insight into this journey, explore our resources on Addiction Recovery Challenges.
Withdrawal in Specific Patient Populations
Different groups require specialized care for opioid withdrawal:
- Pregnant individuals: Abrupt withdrawal is dangerous for the fetus. Maintenance therapy with methadone or buprenorphine is the standard of care to stabilize both mother and baby. Neonatal Opioid Withdrawal Syndrome (NOWS) may occur after birth but is manageable with medical care.
- Adolescents: Require age-appropriate care that involves family and addresses the unique social and emotional factors of their age group.
- Elderly patients: Often have other health conditions and metabolize drugs differently, necessitating slower tapers and careful medication management.
- Patients with co-occurring disorders: Need integrated treatment that addresses both substance use and mental health conditions (e.g., depression, anxiety) simultaneously. Withdrawing from multiple substances, like alcohol or benzodiazepines, requires specialized medical supervision.
The Importance of Aftercare and Continued Support
Detoxification alone rarely leads to lasting recovery. Without ongoing support, the risk of a fatal overdose upon relapse is high due to reduced tolerance.
Effective aftercare is crucial and should include:
- Counseling and Therapy: Individual and group sessions to develop coping skills and address underlying issues.
- Support Groups: Peer communities like Narcotics Anonymous provide accountability and shared understanding.
- Relapse Prevention Planning: Identifying triggers and creating strategies to manage cravings and respond to a lapse.
- Ongoing Medical Care: Continued management of medications and overall health.
Our Opioid Addiction Treatment Program provides this comprehensive, long-term support. As we note in What Happens After Quitting Alcohol, recovery is a marathon, not a sprint. You’ve done the hard work of detox; now it’s time to build a life in recovery.
Frequently Asked Questions about Safe Opioid Withdrawal
Here are answers to some of the most common questions about safe opioid withdrawal.
When should I seek immediate medical help during withdrawal?
While supervised withdrawal is safe, contact your provider or call 911 for severe complications, including:
- Uncontrollable vomiting or diarrhea
- Chest pain or difficulty breathing
- Confusion, disorientation, or hallucinations
- Thoughts of self-harm or suicide
- Seizures (a risk with co-occurring dependencies)
- High fever
Always err on the side of caution and seek help if you are concerned.
What is the biggest risk after completing opioid withdrawal?
The single biggest risk is relapse leading to a fatal overdose. After abstinence, your body’s tolerance to opioids drops significantly. If you use the same amount you did before, your system can be overwhelmed. This danger is amplified by the prevalence of fentanyl in illicit drugs.
To mitigate this risk:
- Have naloxone (Narcan) available and ensure loved ones know how to use it to reverse an overdose.
- Engage in ongoing treatment, including MAT, counseling, and support groups, to prevent relapse.
This heightened risk highlights the need for continued support after a Heroin Detox.
How can I report a problem with my opioid medication?
If you experience a serious side effect or product quality issue with an opioid, report it to the FDA MedWatch program. Your report helps the FDA monitor medication safety.
You can report a problem in several ways:
- Online: Use the FDA MedWatch online portal.
- By Phone: Call 1-800-332-1088 to request a form.
- By Fax: Submit a completed form to 1-800-FDA-0178.
Your Path to a Secure Recovery Starts Here
You’ve taken an important step just by reading this far. Understanding safe opioid withdrawal is the first part of a journey that requires courage, honesty, and support—but you don’t need to walk it alone.
We’ve established that quitting “cold turkey” is dangerous due to severe withdrawal, psychological distress, and the risk of a fatal relapse. Your body needs time and medical support to heal. Medically supervised tapering, combined with Medication-Assisted Treatment (MAT) and holistic support, provides a safe and effective path forward.
Recovery is a long-term journey. Aftercare is essential for managing the post-detox risk of overdose and building a foundation for lasting sobriety.
Safety first. Professional guidance is crucial. Recovery is a journey.
At ARIA Kentucky, we see you as a whole person. Our accredited, certified team provides individualized care, from medically supervised detox to comprehensive outpatient programs. We don’t just help you stop using opioids; we help you build a life worth living.
Your courage brought you here. Let us help you take the next step.
Find a comprehensive prescription drug detox program in Kentucky

