The Emerging Threat Changing America’s Drug Crisis
Tranq is a veterinary tranquilizer called xylazine that’s now infiltrating America’s illicit drug supply at an alarming rate. This powerful animal sedative is being mixed with fentanyl and other street drugs, creating a devastating new chapter in the overdose epidemic.
What You Need to Know About Tranq:
- What it is: Xylazine, a non-opioid sedative approved only for veterinary use in animals like horses and cattle
- Why it’s dangerous: Causes severe sedation, dangerously low blood pressure, slowed breathing, and horrific skin wounds that can lead to amputation
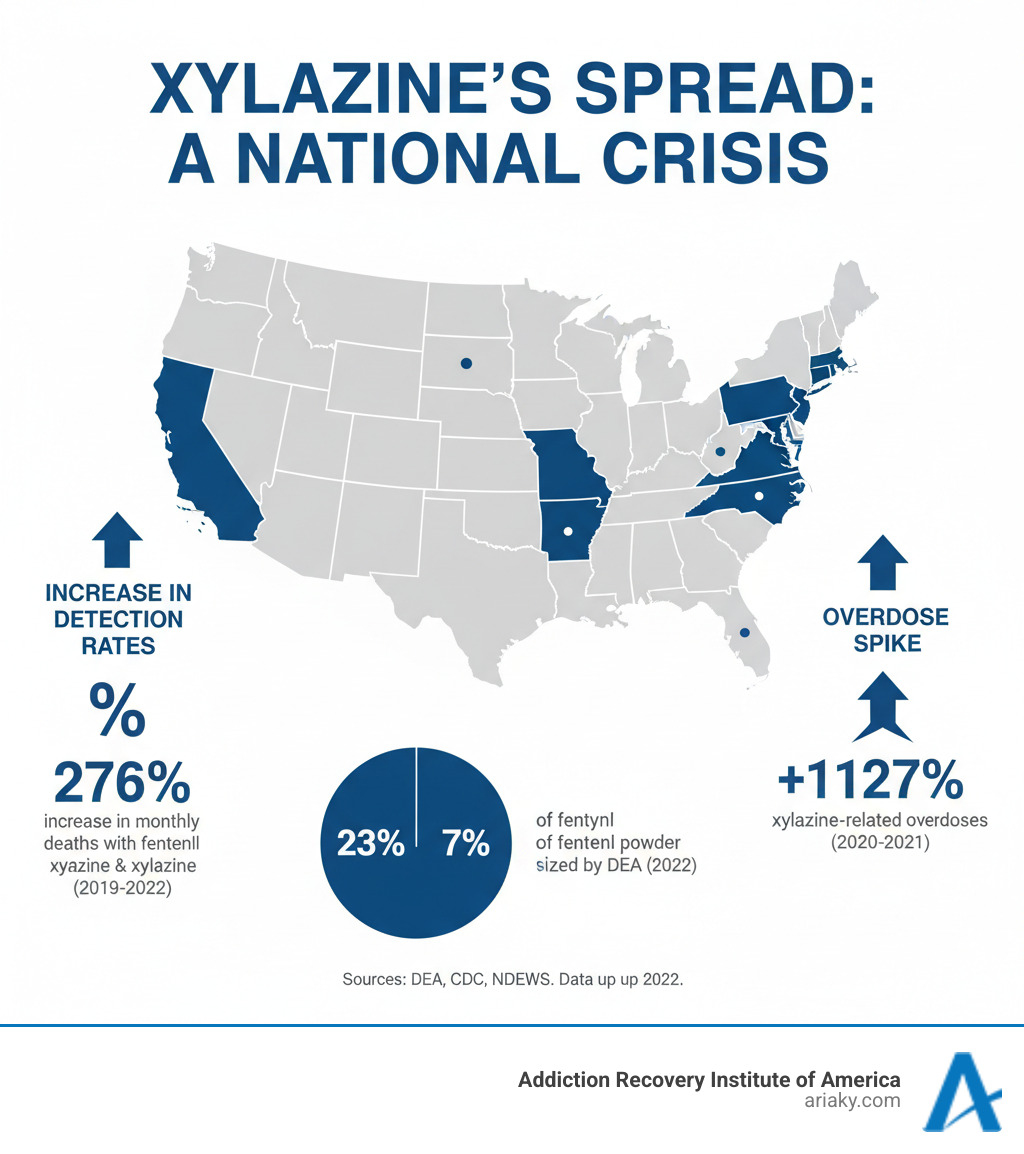
- The alarming spread: Found in 23% of fentanyl powder and 7% of fentanyl pills seized by the DEA in 2022
- Critical limitation: Naloxone (Narcan) cannot reverse xylazine’s effects, though it should still be given for suspected opioid overdoses
- Street names: Tranq, tranq dope, zombie drug, sleep cut
The numbers are sobering: from 2020 to 2021, xylazine-related overdoses increased by as much as 1,127% in some U.S. regions. In Minnesota, fentanyl was found in all seventy tranq-related overdoses between 2019 and 2022.
The White House designated fentanyl mixed with xylazine as an “emerging threat” to the United States in 2023.
Why is tranq so dangerous? This veterinary sedative causes unique complications. Users develop severe skin wounds and tissue death, even without injecting the drug. These wounds can appear anywhere and may require hospitalization or amputation.
For anyone struggling with addiction or worried about a loved one, understanding tranq is now essential for survival.
What is Tranq? The Rise of a Veterinary Sedative
Xylazine—better known on the streets as tranq—was never meant for humans. This powerful non-opioid sedative was developed for veterinary medicine to calm large animals like horses and cattle. It works as a sedative, painkiller, and muscle relaxant, and the FDA approved it strictly for animal use because of its intense effects.
Tranq has escaped veterinary clinics and infiltrated the illicit drug supply. Most users are unaware they’re taking it, as dealers mix it into other substances as a deadly surprise. People encounter tranq through injection, snorting, swallowing, or smoking, depending on the drug it’s mixed with.
Why add a horse tranquilizer to street drugs? Dealers mix tranq with Opiates like fentanyl for several reasons. First, it extends fentanyl’s short high. Adding tranq creates a longer, more sedating experience that mimics the prolonged euphoria of heroin. Second, it’s a cheap cutting agent that bulks up the product, stretching the supply and increasing profits for dealers.
The illicit use of tranq began in Puerto Rico in the early 2000s, where it was called “Anestesia de Caballo” (horse anesthetic). It has since spread across the mainland U.S., including to Kentucky, where its impact is devastating.
Common Street Names for Tranq
Recognizing xylazine’s various street names can help you identify the risks. Common terms include:
- Tranq: Short for tranquilizer.
- Tranq dope: When mixed with opioids.
- Zombie drug: Refers to the disoriented, unresponsive state it induces.
- Anestesia de caballo: The original name, meaning horse anesthetic.
- Sleep cut: Highlighting its powerful sedative properties.
- Horse tranq: A direct nod to its veterinary origins.
The Alarming Health Risks of the Tranq Drug
Tranq is a powerful central nervous system depressant that slows the body to dangerous levels. The sedation is profound and can quickly become life-threatening. It causes dangerously low blood pressure, a dramatically slowed heart rate, and shallow, labored breathing that can lead to organ failure.
When mixed with opioids like fentanyl, these effects multiply, creating a perfect storm that dramatically increases the risk of fatal overdose. We see these cases regularly, and each one reminds us why education about this substance is so critical as part of the broader Substance Abuse Topics we address.

Symptoms of a Tranq-Involved Overdose
Recognizing a tranq-involved overdose is vital. Look for these critical warning signs:
- Completely unresponsive in a state of deep sedation
- Blue or grayish skin, especially around the lips and fingertips
- Dangerously slow or stopped breathing
- Pinpoint pupils
- Cold skin and a faint heartbeat
Naloxone won’t reverse xylazine’s effects, but you should still administer it immediately if you suspect an opioid overdose. Since tranq is almost always mixed with fentanyl, naloxone can reverse the opioid component and save a life. If sedation persists after naloxone, tranq is likely involved. Call 911 right away. Emergency responders can provide oxygen and breathing support. While waiting for help, give rescue breaths. This is critical for tranq overdoses because the drug slows breathing so dramatically.
Severe Skin Wounds: A Devastating Side Effect
A horrifying aspect of tranq use is the devastating skin wounds it causes. These are not typical injection site infections but severe wounds that can appear anywhere on the body. Users develop painful abscesses, deep open ulcers, and necrosis (tissue death). Without treatment, these wounds can lead to amputation.
Disturbingly, these wounds are not limited to injection sites; they also affect people who snort or smoke tranq. The drug appears to reduce blood flow and oxygen to tissues, causing them to die from the inside out. The medical community is still learning to treat these wounds, but basic wound care techniques are crucial. Seek medical attention immediately if these wounds appear.
Xylazine Withdrawal and Addiction Challenges
Tranq withdrawal presents unique and serious challenges. Although not yet an official disorder, people develop dependence on tranq, and withdrawal can be severe and dangerous.
Unlike Heroin Detox, tranq withdrawal causes its own concerning symptoms, including severe irritability and anxiety and a profound sense of unease. Some people also develop a rapid heart rate and dangerously high blood pressure, which can lead to serious cardiac complications.
When mixed with fentanyl, the withdrawal is even more complex. This is why specialized Medical Detox is so important. Detoxing alone can be dangerous. In a supervised setting, providers can monitor vital signs, manage risks, and provide support. Our team creates individualized treatment plans to address the unique effects of xylazine and ensure you get through withdrawal safely.
The Epidemic by the Numbers: Xylazine Statistics and Trends
The spread of tranq is documented in alarming statistics from the Drug Enforcement Administration (DEA), showing how deeply xylazine has infiltrated U.S. communities.
In 2022, the DEA found xylazine in 23% of seized fentanyl powder and 7% of fentanyl pills. These mixtures have been found in 48 of 50 states, making it a national crisis.
The human toll is staggering. Between August 2021 and August 2022, 107,735 Americans died from drug poisonings, with two-thirds involving synthetic opioids like fentanyl. Tranq is an increasing part of this deadly equation.
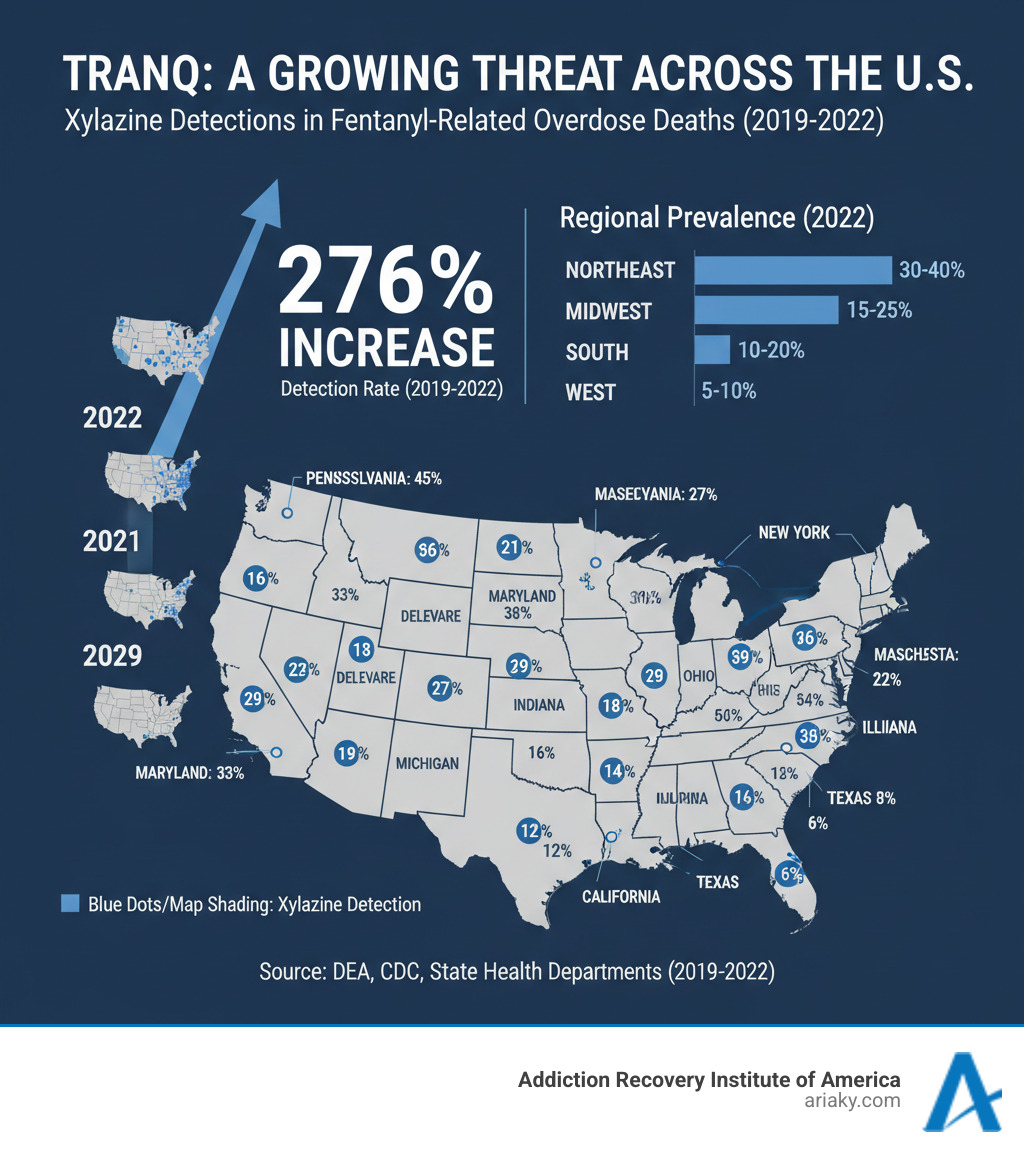
From January 2019 to June 2022, the monthly percentage of fentanyl-involved deaths with xylazine increased by 276%, jumping from 3% to 11%. In some parts of the U.S., xylazine-related overdoses surged by as much as 1,127% between 2020 and 2021 alone.
Regional data shows xylazine is nearly ubiquitous in Philadelphia’s drug supply, with dramatic increases also seen in the Midwest. A multi-city study found xylazine’s involvement in overdose deaths climbed from less than 1% in 2015 to nearly 7% in 2020. In Minnesota, researchers confirmed that fentanyl was present in all seventy tranq-related overdoses between 2019 and 2022, showing these two substances are almost always found together.
Research like the study Illicitly manufactured fentanyl-involved overdose deaths with detected xylazine – United States, January 2019–June 2022 and tracking by organizations like the National Drug Early Warning System (NDEWS) help us understand the scope of this epidemic. These statistics make it clear that tranq has fundamentally changed the overdose crisis, demanding vigilant and effective treatment strategies.
Fighting Back: Harm Reduction, Legal Action, and Recovery
Fighting the tranq crisis requires a multi-front approach, including harm reduction, research, and legal action. The Addiction Recovery Challenges posed by tranq are profound, and recovery ranks among the Hardest Drugs Recovery journeys. But with a coordinated effort, we can create pathways to safety and healing.
Harm Reduction Strategies to Mitigate Risk
For those who use drugs, harm reduction strategies focus on safety and can be life-saving.
- Testing your drugs with commercially available xylazine test strips offers critical information, despite the potential for false positives with some substances.
- Never using alone is a crucial safety step. Services like the Never Use Alone hotline or using with a friend can save a life.
- Carrying naloxone is essential. While it doesn’t reverse tranq, it can reverse the effects of the opioids it’s almost always mixed with, buying time for emergency responders.
- Safer injection practices, such as using sterile equipment and rotating injection sites, reduce harm. The National Harm Reduction Coalition offers detailed guidance.
- Seeking medical care for wounds cannot wait. The skin wounds from tranq can deteriorate rapidly.
- Rescue breaths are especially important when tranq is involved, as it dramatically slows breathing. Providing rescue breaths can keep oxygen flowing until help arrives.
- Good Samaritan laws in most states protect you from arrest when you call 911 for an overdose. Don’t hesitate to call for help.
Government Response and Legal Status
The federal government is responding. In 2023, the White House designated fentanyl with xylazine an emerging threat, leading to a National Response Plan to combat the crisis.
Currently, xylazine is not a federal controlled substance. However, states like Ohio, Pennsylvania, West Virginia, and Florida have moved to add it to their state-controlled substances lists. The FDA has also implemented import restrictions to limit the illicit supply.
The Future of Treatment and Research
The path forward requires better understanding and treatment of tranq addiction, and significant research is underway. The National Institute on Drug Abuse (NIDA) is leading initiatives to track xylazine’s spread, understand its health effects, and develop new treatments, including studying the effect of xylazine on fentanyl addiction.
Researchers are investigating combining naloxone with atipamezole, a veterinary drug that reverses xylazine, to treat overdoses involving both substances. Studies are also focused on treating the severe skin wounds, with early evidence suggesting that keeping wounds clean and open is best for healing.
At ARIA Kentucky, we integrate these emerging insights into our care. Our specialized Tranq Addiction Treatment Program Kentucky reflects our commitment to providing comprehensive support for recovery.
Frequently Asked Questions about Tranq
As tranq spreads, many have urgent questions. Here are answers to the most common concerns.
Can Narcan (naloxone) reverse a tranq overdose?
Naloxone cannot reverse xylazine’s effects. Xylazine is a sedative, not an opioid, so naloxone has no effect on it.
However, you must always give naloxone if you suspect an opioid overdose. Since tranq is almost always mixed with fentanyl, the naloxone can reverse the opioid component and save a life.
If the person remains sedated after naloxone, the xylazine is still active. Call 911 immediately for supportive care. Rescue breaths are critical while waiting for help, as xylazine severely slows breathing.
Are the skin wounds from tranq only caused by injecting it?
No. One of the most unsettling facts about tranq is that the devastating skin wounds can appear regardless of how the drug is used—including snorting, smoking, or swallowing.
The wounds can appear anywhere on the body, not just at a point of contact. This indicates the damage is systemic, likely caused by tranq reducing blood flow and oxygen to tissues, causing them to die from the inside out. These wounds are painful, heal slowly, and can become seriously infected, so seek medical care at the first sign of a lesion.
How can I know if drugs contain tranq?
You can’t tell by looking. The illicit drug market is unregulated, and there is no way to visually identify tranq. Even dealers may not know what their product contains.
The best tool is using xylazine test strips, which are available through harm reduction programs. While not perfect (they can show false positives with some substances), they are a valuable way to reduce risk. Many programs also offer drug checking services.
If you use drugs and notice unusually prolonged sedation or develop any unusual skin lesions, these could be signs that tranq is in your supply. The only way to be certain you’re avoiding tranq is to avoid illicit drugs. When you’re ready for recovery, we’re here to help.
Conclusion: Finding a Path Forward from the Tranq Crisis
The tranq crisis is a wake-up call. This veterinary sedative, mixed with fentanyl, brings devastating consequences: profound sedation, horrifying skin wounds, and complex overdoses. Statistics show its rapid, deadly spread across the country.
But there is hope. Communities are using harm reduction strategies to save lives, the government has designated it an emerging threat, and scientists are developing new treatment approaches.
Most importantly, addiction is a treatable disease. Recovery from substances as dangerous as fentanyl mixed with tranq is possible. We have witnessed people find their way back to health and hope.
At ARIA Kentucky, we understand that every person’s journey is unique. Our specialized programs address the physical, emotional, and psychological components of addiction, and our team stays current with the latest research to provide evidence-based care.
If you or a loved one is struggling, you don’t have to face this alone. The path to sobriety begins with a single step, like reaching out for information. Our Substance Abuse Treatment Complete Guide can help you understand your options.
For those specifically concerned about fentanyl and tranq, we offer specialized support. You can Get help with Fentanyl Detox in Kentucky right here, right now. We’re ready to walk alongside you on your recovery journey.
The tranq crisis is real and dangerous, but it doesn’t have to be the end of anyone’s story. With awareness, support, and compassionate care, recovery is happening every day.



