Understanding the Fentanyl Withdrawal Crisis
A fentanyl detox protocol is a medically supervised plan to safely manage withdrawal symptoms when a person stops using fentanyl. It typically involves medications like buprenorphine, 24/7 monitoring, and symptom management over a 7-10 day acute phase, followed by ongoing treatment.
The fentanyl crisis has reshaped opioid addiction treatment. This synthetic opioid is up to 100 times more potent than morphine and is involved in over 70% of opioid-related deaths in the U.S. In 2021 alone, over 80,000 people died from overdoses involving synthetic opioids like fentanyl.
The good news? Recovery is absolutely possible with the right medical support.
Fentanyl withdrawal is notoriously severe, more so than from heroin or prescription opioids. Its extreme potency and tendency to store in body fat create intense, unpredictable symptoms often described as the worst flu imaginable, compounded by severe anxiety and cravings.
Trying to detox alone is dangerous due to risks of severe dehydration, relapse leading to a fatal overdose, and other unmanaged complications. Medically supervised detox isn’t just recommended—it’s essential for safety and success.
This guide explains what a fentanyl detox protocol involves, the medications used, and why professional treatment is your first step toward lasting recovery.
Fentanyl detox protocol terms made easy:
Understanding Fentanyl Withdrawal: Symptoms, Timeline, and Risks
Fentanyl is a synthetic opioid up to 100 times stronger than morphine, creating profound physical dependence. Its lipophilic nature—meaning it stores in body fat—can cause prolonged and intense withdrawal symptoms when use stops. The severity of withdrawal depends on the dose, duration of use, overall health, and the presence of other substances like xylazine or benzodiazepines, which complicate the process.
Quitting fentanyl on your own is dangerous. Complications like severe dehydration, electrolyte imbalances, and aspiration pneumonia are serious medical risks. The intense discomfort also makes relapse highly likely. After even a few days of abstinence, tolerance drops, meaning a relapse on a previous dose can be fatal. This is why a medically supervised fentanyl detox protocol is critical.
Common Physical and Psychological Symptoms
Fentanyl withdrawal affects both body and mind. Physical symptoms are severe and include:
- Nausea, vomiting, and diarrhea, leading to dehydration.
- Deep muscle and bone aches.
- Sweating, chills, and goosebumps.
- Racing heart (tachycardia) and high blood pressure.
- Insomnia and exhaustion.
The psychological symptoms can be even more challenging:
- Intense, overwhelming cravings for fentanyl.
- Severe anxiety, agitation, and panic attacks.
- Deep depression and feelings of hopelessness.
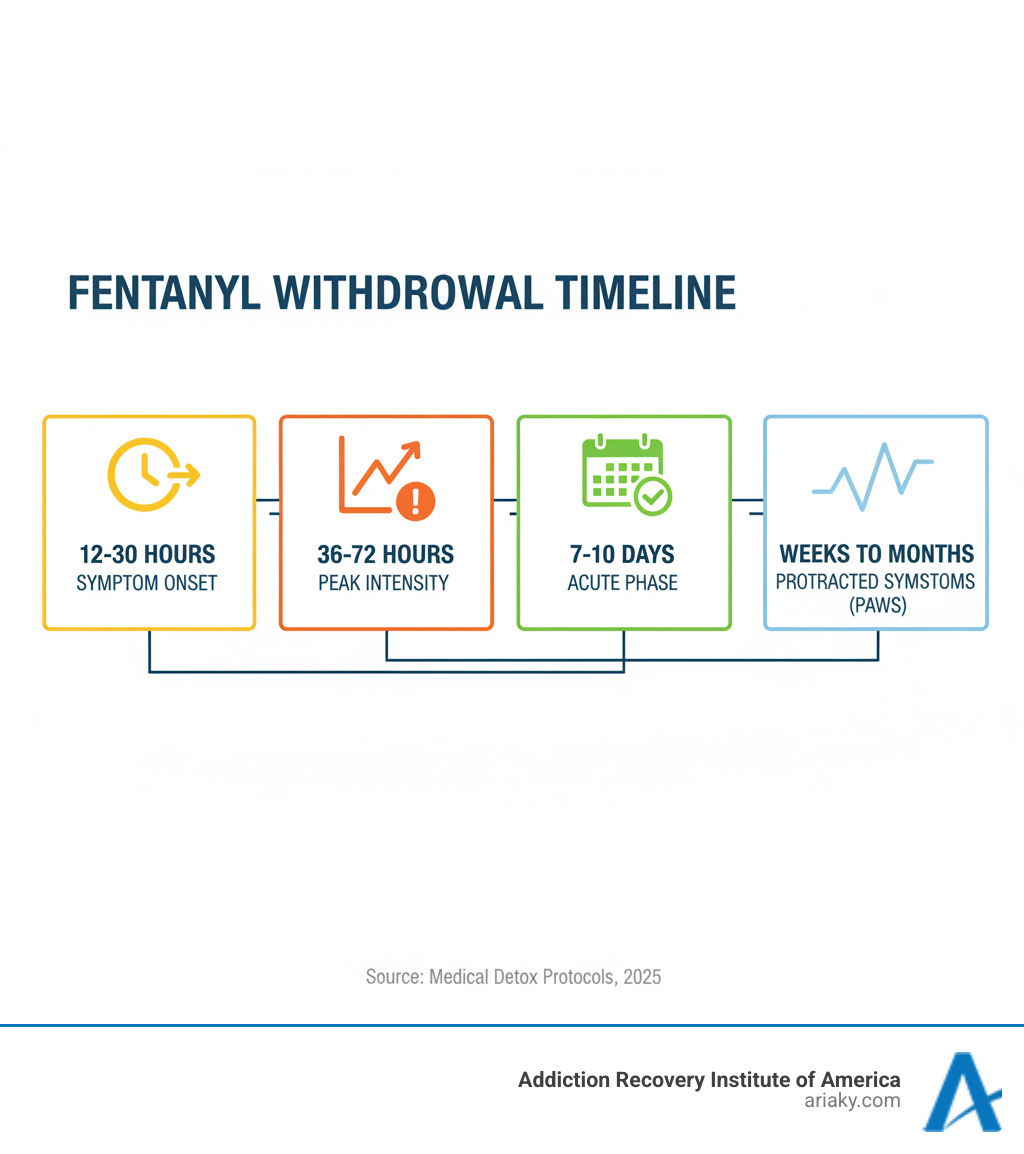
The Typical Timeline for Fentanyl Withdrawal
While individual experiences vary, a general timeline helps set expectations:
- Onset (12-30 hours after last use): Early symptoms like anxiety, restlessness, and muscle aches begin.
- Peak (36-72 hours): Symptoms reach their highest intensity. This is the most difficult phase, where medical support is crucial.
- Acute Phase (7-10 days): The most severe physical symptoms gradually subside.
- Post-Acute Withdrawal Syndrome (PAWS): Lingering psychological symptoms like anxiety, depression, and cravings can persist for weeks or months.
How Fentanyl Withdrawal Differs from Other Opioids
Fentanyl withdrawal is generally more severe than with other opioids. Its high potency leads to more intense symptoms. Because it stores in body fat, withdrawal can have an unpredictable course, sometimes with symptoms worsening after a brief improvement. This also creates a higher risk of precipitated withdrawal when starting buprenorphine (Suboxone), requiring specialized induction protocols.
Compared to heroin, fentanyl withdrawal is often more intense. Compared to methadone, which has a longer-acting profile, fentanyl withdrawal starts faster and is more acute, though the acute phase is typically shorter.
Potential Complications and How They’re Managed
Medical supervision is key to managing potentially dangerous complications:
- Dehydration and Electrolyte Imbalance: Managed with IV fluids and monitoring to prevent cardiac issues.
- Aspiration Pneumonia: Prevented with anti-nausea medication and close observation.
- Severe Anxiety and Panic: Eased with comfort medications in a calm, supportive environment.
- Suicidal Ideation: The intense depression can lead to thoughts of self-harm. Our team provides constant emotional support and monitoring. If you or someone you know is in crisis, call or text the 988lifeline.org immediately.
A Medically Supervised Fentanyl Detox Protocol

A professional fentanyl detox protocol is about managing withdrawal safely, preventing complications, and preparing you for long-term recovery. Our approach follows the evidence-based guidelines from the American Society of Addiction Medicine (ASAM), which you can learn more about at samhsa.gov/resource/ebp/asam-national-practice-guideline-treatment-opioid-use-disorder. Medical detox is the essential first step for anyone physically dependent on opioids.
Key Elements of a Fentanyl Detox Protocol: Medications Used
Medication-Assisted Treatment (MAT) is the cornerstone of fentanyl withdrawal management. It uses FDA-approved medications to reduce withdrawal symptoms and cravings.
- Buprenorphine (e.g., Suboxone): A partial opioid agonist that eases withdrawal and cravings without a dangerous high. Starting it requires careful timing to avoid precipitated withdrawal.
- Methadone: A full opioid agonist that has been used for decades. It effectively blocks cravings and withdrawal symptoms.
- Lofexidine (Lucemyra): A non-opioid medication that calms the nervous system to reduce physical symptoms like muscle aches and anxiety, but does not address cravings.
- Clonidine: Another non-opioid that helps with physical symptoms like anxiety, sweating, and restlessness.
- Comfort Medications: We also use medications to manage specific symptoms like nausea, diarrhea, and insomnia.
Here’s how the primary medications compare:
| Medication | Type | How it Works | Fentanyl Detox Specifics | Retention Rates (General OUD) |
|---|---|---|---|---|
| Methadone | Full Opioid Agonist | Blocks cravings, alleviates withdrawal symptoms, prevents euphoria from other opioids | Requires careful titration, can be started at higher doses for fentanyl users (e.g., 30mg initial, 100+mg for maintenance) | 73.9% at 4 months, 74.0% at 6 months |
| Buprenorphine (e.g., Suboxone) | Partial Opioid Agonist | Eases withdrawal symptoms and cravings, has a ceiling effect for respiratory depression | Induction can be challenging due to precipitated withdrawal; microdosing or other modified protocols may be used | 45.9% at 4 months, 46.0% at 6 months |
| Lofexidine (Lucemyra) | Non-Opioid Alpha-2 Adrenergic Agonist | Reduces physical withdrawal symptoms (e.g., muscle aches, sweating, anxiety) by lowering norepinephrine | Does not address cravings, often used as an adjunct or for individuals who cannot or prefer not to use opioid agonists | Not applicable (symptomatic relief only) |
The Role of Buprenorphine and Methadone in a Fentanyl Detox Protocol
Buprenorphine and methadone are central to a fentanyl detox protocol because they activate the same brain receptors as fentanyl in a controlled way, reducing withdrawal and cravings. Fentanyl’s potency creates challenges, especially the risk of precipitated withdrawal with buprenorphine. To prevent this, we use specialized approaches like microdosing (gradually introducing buprenorphine) to ensure a smooth transition.
Methadone is often an effective option for those with high fentanyl tolerance, as it can be increased to a therapeutic dose more quickly. Research shows that fentanyl users often require methadone doses of 100mg or higher to manage symptoms effectively. Both medications are proven to keep people in treatment, and the best choice depends on your individual needs.
Choosing the Right Setting: Inpatient vs. Outpatient Detox
Choosing the right setting is crucial for safety and success.
Inpatient detoxification is the recommended standard for fentanyl withdrawal. It is ideal for those with heavy or prolonged use, polysubstance use, co-occurring health conditions, or an unstable home environment. Our inpatient facilities in Kentucky provide 24/7 medical supervision in a trigger-free environment, offering the safest and most comfortable detox experience. ARIA Kentucky has inpatient services in Ashland, Bowling Green, Florence, Lexington, Louisville, Morehead, Newport, Owensboro, and Paducah.
Outpatient detoxification may be an option for individuals with a shorter history of use, a strong support system, and no significant co-occurring conditions. It involves daily or frequent appointments for monitoring and medication. However, given the intensity of fentanyl withdrawal, inpatient care is generally the safer and more effective choice.
If you’re unsure which setting is right for you, our team can help you choose the safest option for your needs. Visit https://ariaky.com/ to learn more.
Beyond Detox: The Path to Long-Term Recovery
Detox is the necessary first step, but it’s not the end of treatment. A medically supervised fentanyl detox protocol breaks the cycle of physical dependence, but it doesn’t address the underlying reasons for addiction. Lasting recovery requires healing the emotional wounds, learning new coping skills, and changing the thought patterns that led to substance use.
Think of detox like setting a broken bone—it stabilizes the immediate problem, but physical therapy is needed to regain full function. Without continued treatment after detox, relapse rates are dangerously high. A relapse after detox is especially deadly because your tolerance has dropped, dramatically increasing the risk of a fatal overdose.
Our approach treats the whole person, helping you heal from underlying trauma, co-occurring mental health disorders like depression or anxiety, and relationship issues. We focus on building effective relapse prevention strategies to give you the tools for a new life in recovery.
The Importance of a Comprehensive Treatment Plan
Recovery is not one-size-fits-all, so we create individualized treatment plans that combine several therapeutic approaches.
- Individual and Group Therapy: Individual therapy helps you explore the root causes of your addiction in a private setting. Group counseling provides peer support and connection, reducing the isolation that often accompanies addiction.
- Family Therapy: Addiction affects the entire family. Therapy helps mend relationships, improve communication, and educate loved ones on how to provide effective support.
- Dual Diagnosis Treatment: Many people with opioid use disorder also have co-occurring mental health conditions like anxiety or PTSD. We treat both simultaneously for the best chance at lasting recovery.
- Cognitive Behavioral Therapy (CBT): This evidence-based therapy helps you identify and change negative thought patterns and behaviors related to substance use, teaching practical skills for managing cravings and high-risk situations.
Our residential treatment services in Kentucky provide a structured environment where these therapies are integrated into your daily life. Learn more about our residential treatment services at https://ariaky.com/.
Follow-Up Care and Long-Term Implications
Transitioning back to daily life can be challenging, which is why follow-up care is a core part of our treatment plans.
- Aftercare Planning: Before you leave our program, we create a personalized plan that includes ongoing therapy, support group meetings, and sober living arrangements if needed.
- Sober Living and Support Groups: Sober living homes offer a structured, drug-free environment to bridge the gap between residential treatment and independent living. Support groups like Narcotics Anonymous and SMART Recovery provide invaluable, ongoing peer encouragement.
- Ongoing Medication-Assisted Treatment (MAT): Continuing buprenorphine or methadone long-term significantly reduces the risk of relapse and overdose. It is a proven medical approach that supports stability while you rebuild your life.
Our Intensive Outpatient Programs (IOP) offer flexible, structured support as you transition back to your community, allowing you to practice new skills in a real-world setting. Explore our Intensive Outpatient Program (IOP) services at https://ariaky.com/.
Lasting sobriety is a journey. With comprehensive treatment and ongoing support, it is within your reach. For more information, visit https://ariaky.com/.
How Fentanyl Withdrawal Compares to Other Substances
Understanding how fentanyl withdrawal differs from other substances highlights why a specific fentanyl detox protocol is necessary. Each substance impacts the brain differently, leading to unique withdrawal symptoms and risks.
Opioids like fentanyl affect the opioid receptor system, causing severe flu-like symptoms and psychological distress. In contrast, alcohol and benzodiazepines affect the GABA system, while stimulants like methamphetamine impact dopamine. These different pathways create distinct withdrawal experiences.
The most critical difference is the level of medical risk. While fentanyl withdrawal is uncomfortable and has risks from complications, withdrawal from alcohol or benzodiazepines can be directly life-threatening.
Fentanyl vs. Alcohol & Benzodiazepines
Withdrawal from alcohol and benzodiazepines can be fatal and must be medically managed. Abruptly stopping these substances can lead to life-threatening complications that do not occur with opioid withdrawal alone.
- Seizures: Can occur within 12-48 hours after the last use.
- Delirium Tremens (DTs): A severe condition with confusion, hallucinations, and fever that can be fatal without treatment.
For this reason, anyone dependent on these substances requires a gradual medical taper, usually with a long-acting benzodiazepine, to prevent these outcomes. In cases of polysubstance use, managing alcohol or benzodiazepine withdrawal is the first priority.
Fentanyl vs. Stimulants, Cannabis, and Inhalants
Withdrawal from stimulants (methamphetamine, cocaine), cannabis, and inhalants is primarily psychological.
- Stimulant Withdrawal: Characterized by crushing fatigue, severe depression, anxiety, and intense cravings. While not physically dangerous in the same way as opioid withdrawal, the psychological distress can be overwhelming and may lead to suicidal thoughts.
- Cannabis and Inhalant Withdrawal: Symptoms are generally milder and may include irritability, anxiety, and sleep problems. While less intense, psychological dependence can still be strong and benefit from professional support.
In summary, while fentanyl withdrawal is a severe physical and psychological ordeal, alcohol and benzodiazepine withdrawal pose a direct threat to life. Stimulant withdrawal is a battle against profound psychological symptoms. Our comprehensive programs are equipped to manage all types of substance withdrawal safely.
Frequently Asked Questions about Fentanyl Detox
Is fentanyl withdrawal life-threatening?
While fentanyl withdrawal itself is rarely fatal, its complications can be. The primary dangers are:
- Medical Complications: Severe dehydration from vomiting and diarrhea can lead to heart or kidney failure. Aspiration pneumonia is another serious risk.
- Fatal Overdose on Relapse: After detox, your tolerance drops significantly. Relapsing on your previous dose can easily be fatal. This is the single greatest danger.
- Co-occurring Substance Withdrawal: If you are also dependent on alcohol or benzodiazepines, withdrawal can cause deadly seizures or delirium tremens (DTs).
For these reasons, medically supervised detox is essential.
How long does it take to detox from fentanyl?
The acute phase of fentanyl withdrawal typically lasts 7 to 10 days. Symptoms usually begin 12-30 hours after the last dose and peak in intensity around 36-72 hours. After the acute phase, some people experience Post-Acute Withdrawal Syndrome (PAWS), where psychological symptoms like anxiety, depression, and cravings can linger for weeks or months. The exact duration depends on factors like usage history, dose, and individual metabolism.
Can you detox from fentanyl at home?
No. Attempting to detox from fentanyl at home is extremely dangerous and strongly discouraged. The physical and psychological symptoms are often too severe to manage without medical help, leading most people to relapse. As mentioned, relapsing after a period of abstinence is incredibly dangerous due to reduced tolerance.
A medically supervised fentanyl detox protocol provides 24/7 monitoring, medications to ease symptoms, and a safe environment free from triggers. It is the only way to ensure you get through withdrawal safely and successfully.
Conclusion: Your First Step Towards Lasting Sobriety
The journey out of fentanyl addiction is challenging, but recovery is absolutely possible with the right support. You do not have to face it alone.
This guide has shown why a medically supervised fentanyl detox protocol is not just a recommendation—it’s essential for your safety. The risks of detoxing alone, from severe medical complications to a fatal overdose upon relapse, are too high.
Professional help provides the medical monitoring, medications, and emotional support needed to steer withdrawal safely and build a foundation for a new life. At Addiction Recovery Institute of America (ARIA), we provide personalized care that addresses your unique story and challenges.
With locations across Kentucky—including Ashland, Bowling Green, Covington, Florence, Lexington, Louisville, Morehead, Newport, Owensboro, and Paducah—our compassionate, accredited, and AODE-certified team is ready to help.
Taking the first step is the hardest part, but it’s where hope begins. You don’t need to have all the answers; you just need to be willing to reach out.
If you or a loved one is struggling, please don’t wait. Your journey to sobriety can start today. Visit https://ariaky.com/ to learn more about our addiction treatment programs.